General considerations
1. Introduction
Current standards of care for trauma patients, whether polytrauma or isolated craniomaxillofacial injuries, follow the Advanced Trauma Life Support (ATLS) protocol relating to Airway, Breathing, Circulation, Disability, and Environment in that sequence. In the polytrauma patient, on admission, some lesions take higher priority than the craniomaxillofacial lesions. The attending emergency specialist should have detailed information regarding the mechanism of injury as it gives clues about associated and sometimes occult injuries, eg:
- Car ejection injury: suspect C-spine injury, chest trauma, abdominal injury
- Fall from three meters or higher: suspect pelvis and long bone injuries
- Antero-posterior crashing/deceleration trauma: suspect chest injuries, viscera/organs (major vessels can avulse)
Craniomaxillofacial trauma always implies a geographic injury to the head, face, and neck. Head injuries and cervical spine injuries must always be excluded before any craniomaxillofacial treatment is undertaken.
Craniomaxillofacial injuries need to be diagnosed, and a treatment plan must be established and fitted into the total treatment plan for the patient, at an early stage.
The patient’s general medical condition, eg, chest infection, acute respiratory distress syndrome, sepsis, multiple organ failure, associated injuries (cranial, chest, abdomen, fractures of long bones with vascular injury), and age may be a reason for deviation from the principles suggested in this module of the AO Surgery Reference.
The spectrum of midfacial fractures has significantly changed over the last decades. Depending on the socio-economic, geographical, and environmental specifics, the attention towards occupational health and safety, education and prevention, protection measures (eg, in automotive vehicles and sports, etc), and awareness of individuals to prevent injuries has increased. A good example is that the classical dish face lesion frequency has been drastically reduced in car accidents because of the use of seat belts, airbags, and shock-absorbing materials in steering wheels and dashboards.
Particularly in midfacial fracture repair, Paul Manson’s quote: “You never get a second chance.” must be kept in mind, ie, the time frame regarded appropriate for primary fracture treatment is limited to two weeks. As soon as the general condition of the patient allows, definitive treatment should be undertaken. After two weeks, the treatment is regarded as delayed and must follow the protocol of secondary post-traumatic reconstruction. Secondary reconstruction is not a current focus of the AO CMF Surgery Reference.
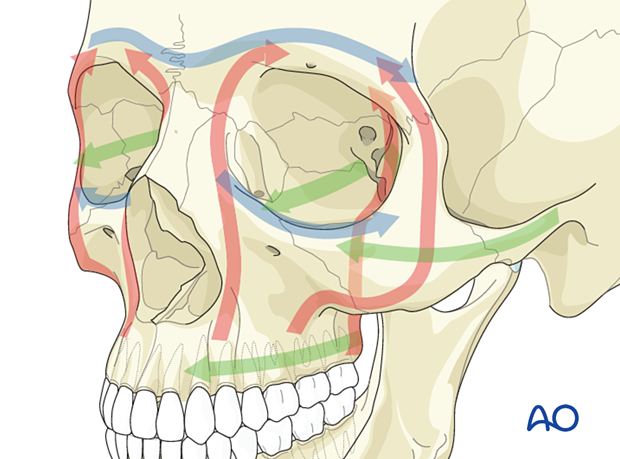
It is not so much the fracture morphology in the midfacial area that limits the intended treatment but mainly the preexisting general health status and the severity of associated injuries in the vicinity of the midface (optic nerve trauma, CSF leakage, bleeding, etc). Regardless of the severity and possible variety of fracture types in the midfacial area, the guideline for successful restoration of midface injuries is reconstructing facial buttresses and prominences, recontouring bony cavities (eg, orbit), and reestablishing the pre-morbid occlusion.
Triage
According to triage, the treatment urgency can be categorized as follows:
- Immediate treatment: Hemorrhage control, surgical airway for midface fractures, lateral canthotomy for retrobulbar hemorrhage with excess ocular pressure
- Treatment within a few hours: Heavily contaminated wounds, extraoral open fractures
- Treatment can wait for 24 hours: Simple, aseptic fractures
- Treatment can wait for more than 24 hours: hemodynamically unstable patients
2. Fracture classification
The Le Fort classification is a historic classification still widely used to classify midfacial fractures. This classification is based on experiments where cadavers were exposed to frontal impacts. This was one of the first experimental trials on maxillofacial trauma. The cadavers were dissected and analyzed after their injury, and the Le Fort I, II, and III fracture patterns were derived.
Apart from the Le Fort classification, the Markowitz classification describes injury patterns in NOE fractures. Other classifications apply to frontal bone, zygomatic, orbital, and mandibular fractures.
The unique situation of the midface is the complexity of the interaction of hard and soft tissue. Out of twelve cranial nerves, six address the orbital area (CN II, III, IV, V, VI, and VII). Furthermore, in the midface, form, function, and esthetics are interdependent; even minor dislocations may be evident to everyone.
The complexity or simplicity of a fracture in the midface is based not only on the fracture morphology (ie, fragment size, number, dislocation) but also on the degree of injury to the soft-tissue envelope.
The range of combined midfacial/panfacial fractures is enormous. This is due to the variety of possible mechanisms which occur during impact leading to the midfacial injury. In general, low-energy trauma less often leads to severe midfacial fractures than high-energy trauma.
3. Imaging
With the availability of modern imaging technologies, the imaging analysis of the individual fracture pattern shows a variety and complexity that does not always conform to the above-mentioned historical classifications. Today’s gold standard for assessing a particular fracture pattern is voxel-based 3D data sets (CT and cone-beam CT). It is strongly advised to consider postoperative CT scans to determine the surgical result, especially if there is question about the procedure. Because of the enormous benefit of CT documentation and the further development of cone beam technology, more and more surgeons are now recommending intraoperative imaging to assess proper reduction and implant positioning. The scientific literature shows improved outcomes for patients treated for orbital fractures when intraoperative imaging is used. As a result, postoperative imaging and the morbidity of revision surgery can be avoided.
Examination of the craniofacial skeleton vastly benefits from both 2D and 3D imaging and interactive image analysis. The modern surgeon should be trained to use the DICOM voxel data set for multiplanar and 3D image analysis. Various DICOM viewers can be freely downloaded from the internet and used to interact with the DICOM data set to diagnose and plan treatment. (Click here for a list of freely available healthcare software, including DICOM viewers). This is the only way to unlock the barrier interface of filtered information between radiologists and surgeons. The modern surgeon should use complete radiological information and not a limited selection of printouts or digitized views.
Having implemented computer assisted fracture assessment, much more detailed preoperative information is available to the surgical team. Radiological information acquired intraoperatively can be compared with different data sets (obtained pre- and postoperatively) via image fusion.
If no adequate visualization software for the DICOM datasets is available, then CT axial, coronal, and oblique parasagittal views of the midface for simple fractures, with 3D views for more complex fractures, are recommended.
Plain x-rays should only be considered appropriate if CT is unavailable or if specific information for hard-tissue structures involved, such as dentition (dental x-ray, orthopantomogram (OPG)), is required. MRI, CT angiogram, MR angiogram, or ultrasound can be helpful in some specific questions related to soft-tissue or vascular evaluation but is, in most cases, not included in standard diagnostic workup (one exception is optic nerve sheath hematoma detection).
4. Biomechanics of the midface
Introduction
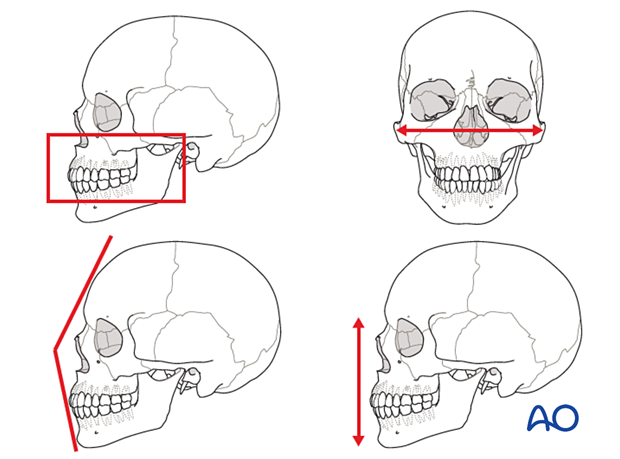
The midface equates to a tent, where the tent poles represent the bony midface, and the tarpaulin represents the overlying soft tissues. However, the vectors of the midface address all three dimensions, ie, vertical, sagittal, and transverse, which makes it much more demanding than the construction plan of a tent.
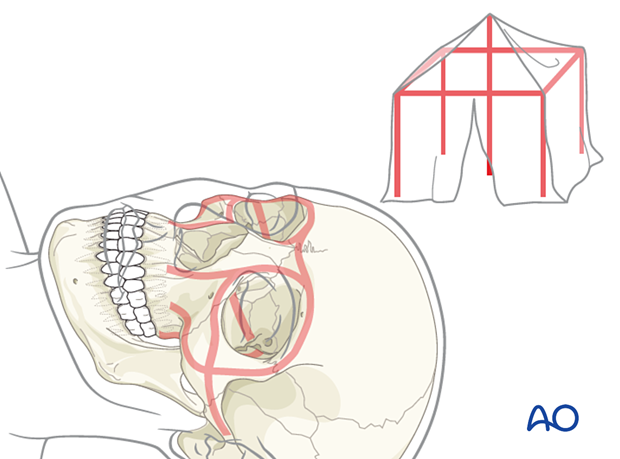
The reconstruction sequence to reestablish midfacial pillars and dimensions begins with establishing the most reliable reference structures. This can be the patient’s occlusion, an outside-to-inside approach (“Joe’s outer frame,” Gruss), or a top to bottom approach as a first step. Manson has described an anatomic unit assembly dividing the face into regions and individual components and assessing each for degree of injury to determine the amount of exposure and fixation required for each sub area. Facial reconstruction can begin in any of the major units according to priority, such as cranial or brain injury. Each unit is managed, and the face is serially assembled.

Every under- or over-contouring of the bony midface in primary fracture repair will likely result in an unfavorable projection of the overlying soft-tissue, and in an esthetic compromise. In addition, functional disorders, such as malocclusion or orbital dysfunction, or an unfavorable appearance may follow.
5. Principles
Airway
Intraoperative MMF necessitates nasotracheal intubation or placing the tube through a gap in or behind dentition. If nasotracheal or oral intubation is not feasible, submental/submandibular intubation or tracheostomy should be considered.
Surgical principles
Dental occlusion is the most critical parameter in reestablishing facial contour, reducing the fracture, and obtaining postoperative chewing function. The most common means of placing the patient into maxillomandibular fixation (MMF) is the application of arch bars. Click here for further details on applying MMF/IMF. Maxillary fractures must be able to be freely repositioned and stabilized to prevent further displacement. The best solution to a displaced nonmobile impacted or incomplete fracture is often to complete the fracture or to release the impaction by osteotomy. Various instrumentations have also been used to achieve the proper position and free movement of the maxilla. Instrumentation that has been used includes Rowe’s disimpaction forceps, the “Stromeyer” hook, and Tessier retromaxillary mobilizers.
A fundamental surgical principle is to achieve correct height, width, and projection of all midfacial bones. The correct anatomical positioning of all midfacial bones must be achieved. Successful reconstruction of midfacial fractures is obtained by reestablishing the midfacial buttresses. If available, old dental records or models and X-rays, may be helpful. Dental casts, stereolithographic models, and premorbid photographs are always helpful guides for treatment.
As a general principle, all fractures should be exposed and reduced before plating.
The midfacial region is possibly the most demanding region for surgical reconstruction and one of the most controversial regions for providing appropriate reconstruction.
It is up to the individual surgeon to determine the appropriate treatment protocol for each patient, including selecting proper hardware for fracture fixation.
The complexity of fracture fixation is determined by fracture morphology, including the number of fracture lines, and depends on the necessary approach, accessibility, visibility of the area of interest, and the stability of the fracture reduction.
The number, size, and position of plates and screws may vary according to biomechanical needs and individual fracture situations.
The use of a plastic skull model in a sterile plastic bag, or the use of sterile artificial skulls for contouring plates, and technologies such as intraoperative imaging or navigation can be beneficial in restoring the proper anatomical form. More recently, the use of computer-assisted surgical planning and 3D-printed patient-specific implants has become more widely adopted.
Pre- and postoperative 2D or 3D imaging allows an objective assessment of the surgical result.