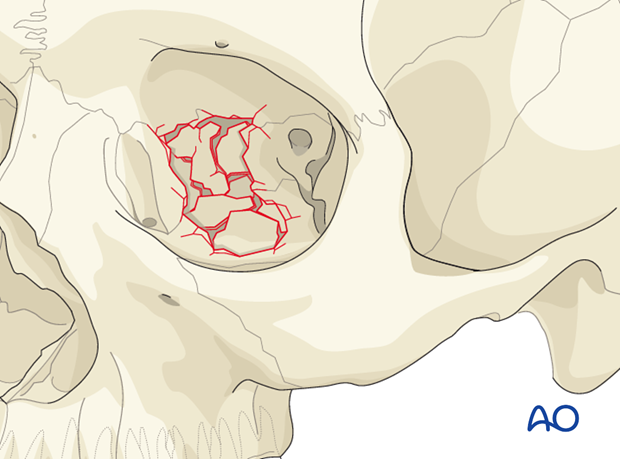
Orbit, combined fracture
Introduction
This is the most frequent orbital wall fracture pattern leading to functional and aesthetic problems.
Clinical diagnosis is based on meticulous examination of the eye, including patient vision and palpation of the orbital aperture.
Prior to CT imaging, 2-D x-rays were considered sufficient for pre- and postoperative diagnostics in orbital fractures. One of the great weaknesses of 2-D imaging is that in many cases a fracture is revealed, but not the degree of fracture displacement. Since the advent of CT imaging, the surgeon can better define fractures, as well the degree of fracture displacement and the necessity for fracture reduction.
The complexity of an orbital fracture is defined by the combination of its anterior-posterior and mediolateral extensions. This complexity is not visible on 2-D x-rays. Therefore, proper diagnosis and treatment should be based on voxel-based datasets (CT, cone beam).
A common feature of an orbital wall fracture is intra-/periorbital air which appears clinically as emphysema (independent of whether the injury was penetrating or nonpenetrating).
The most widely available technology is CT scanning which has the advantage of combined hard- and soft-tissue visualization. Cone beam technology is becoming increasingly popular although only hard tissues can be reliably assessed. MRI is limited to soft-tissue visualization with only indirect information on hard tissues, and is not part of the standard work-up of orbital fractures.
In some cases, radiographic assessment alone is insufficient to determine the extent, morphology, and quality of the fracture. In some complex cases a complete understanding of the fracture morphology is obtained only after surgical exposure.
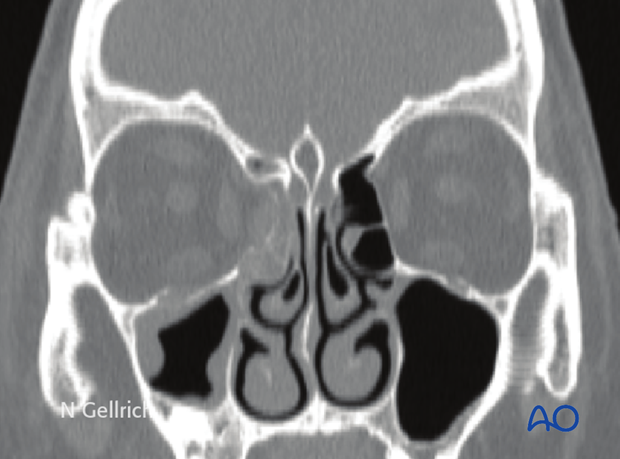
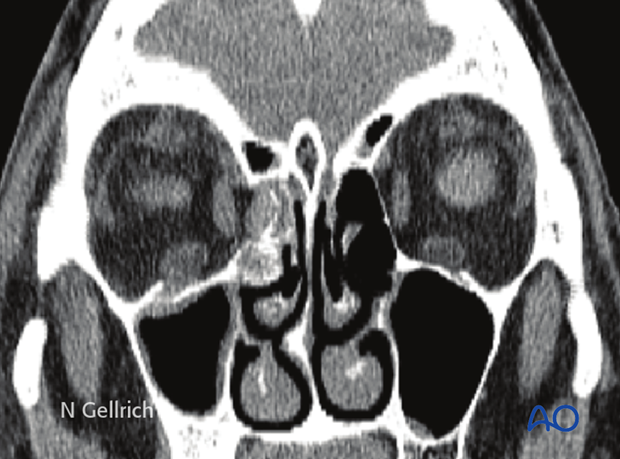
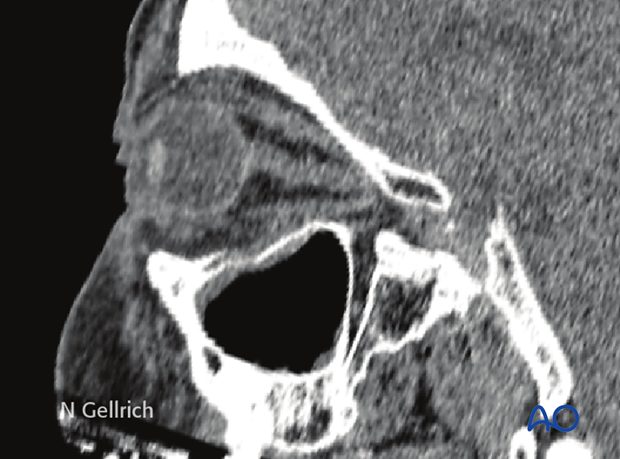
Radiographic findings
Coronal slices (hard-tissue window) of a combined right medial orbital wall and orbital floor fracture.
Coronal slices (soft-tissue window) of a combined right medial orbital wall and orbital floor fracture.
Sagittal slices (soft-tissue window) of the same patient.
Note: A sagittal view for visualization of the orbital floor has to be oriented in the axis of the optic nerve. Then, the plane can be shifted medially and laterally to fully assess the defect in the sagittal plane.
Axial slices (soft-tissue window) of the same patient.














