Upper-eyelid approach
1. General considerations
The upper-eyelid approach, also called upper blepharoplasty, upper-eyelid crease, and supratarsal fold approach is direct and usually aesthetically acceptable.
If there is no natural crease in the supratarsal fold lending itself for the incision line, the upper-eyelid approach follows either the lower or upper limb of an elliptic upper blepharoplasty incision.
2. Anatomy
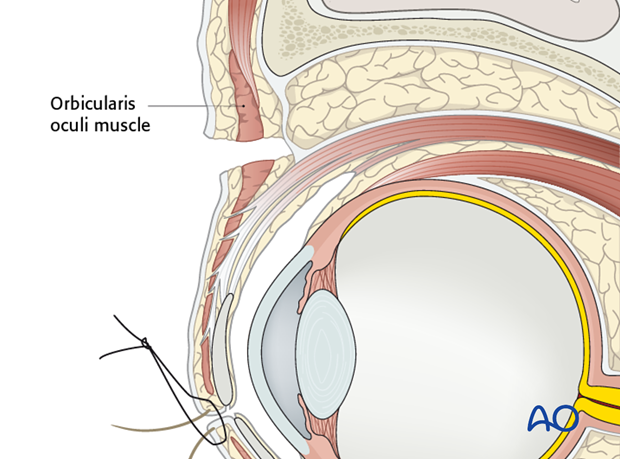
The passageway to the superolateral orbital rim leads from the skin incision through the orbicularis oculi muscle layer.
Skin muscle flaps are raised leaving the orbital septum intact. The preaponeurotic space and the fat pads inside are not entered and serve as a buffer for critical underlying structures such as the levator aponeurosis. Gentle upward and lateral (temporal) traction of the wound edges facilitates access to the supraperiosteal plane over the lateral bony rim rapidly.
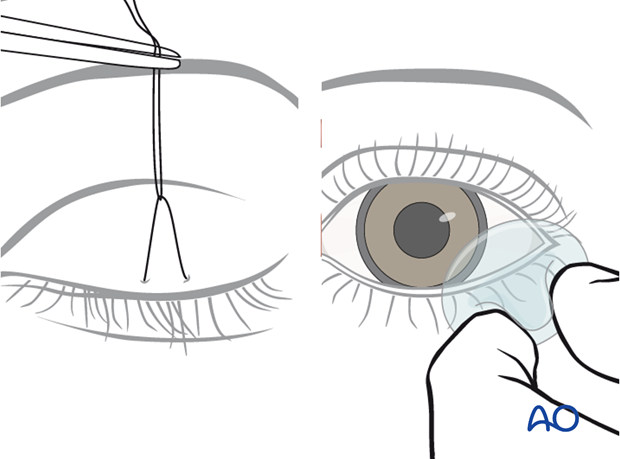
3. Protection of the Globe
The cornea is protected with a temporary tarsorrhaphy (click here for a detailed description of coronal protection) or with a transparent corneal cover shield allowing undisturbed observation of the eye during surgery.
4. Identification and marking of incision line
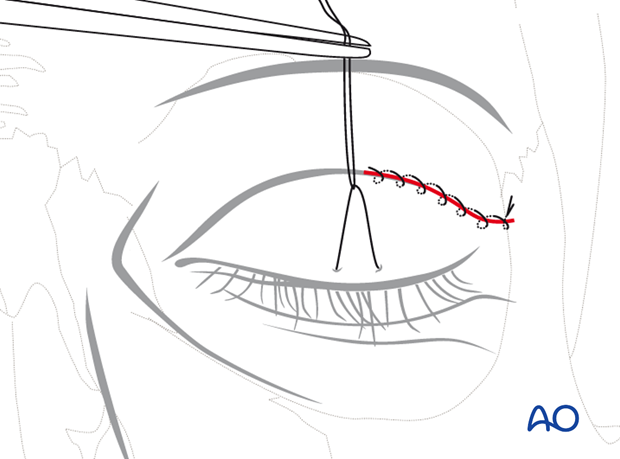
The skin incision in the lateral (temporal) half of the upper lid is designed in a curvilinear fashion with the medial portion being convex superiorly and the lateral portion in line with the lateral canthus. Most appropriately the incision is placed into a natural supratarsal skin crease.
If a lid fold is not detectable the incision line is determined according to the measurements of the lower edge of a standard upper blepharoplasty: 10 mm above the lash line in the central part of the lid and 6-7 mm above the lateral canthus.
The incision may be extended laterally onto the lateral orbital rim then upwardly inclining to improve the surgical access.
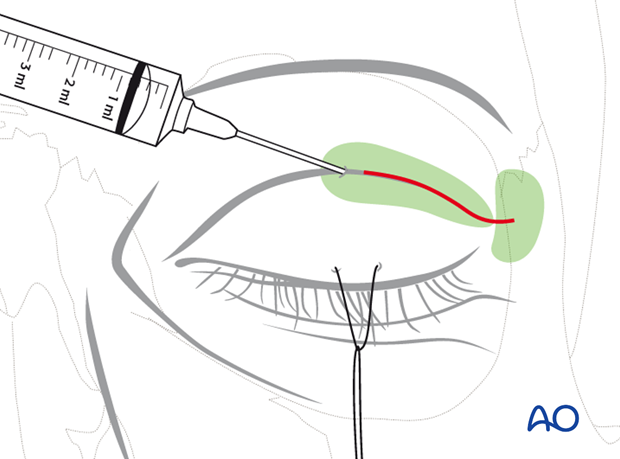
Skin marking is performed prior to infiltration with a vasoconstrictor, which leads to distortion of the tissues.
5. Vasoconstriction
The upper-eyelid skin can be infiltrated with a mixture of local anesthesia and a vasoconstrictor as well as in the supraperiosteal plane over the superolateral orbital rim to be surgically exposed. Adequate time for hemostasis must elapse before procedure.
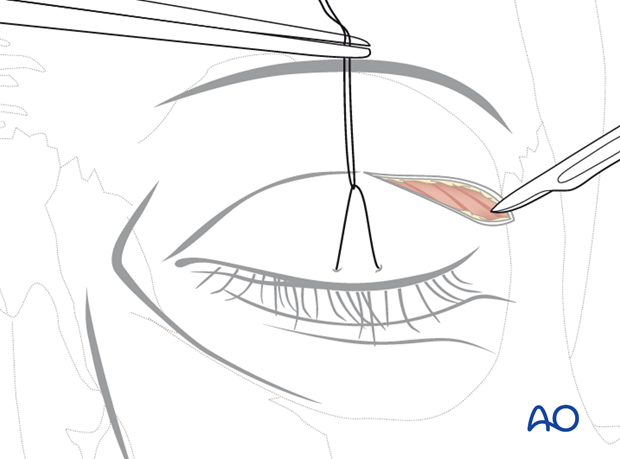
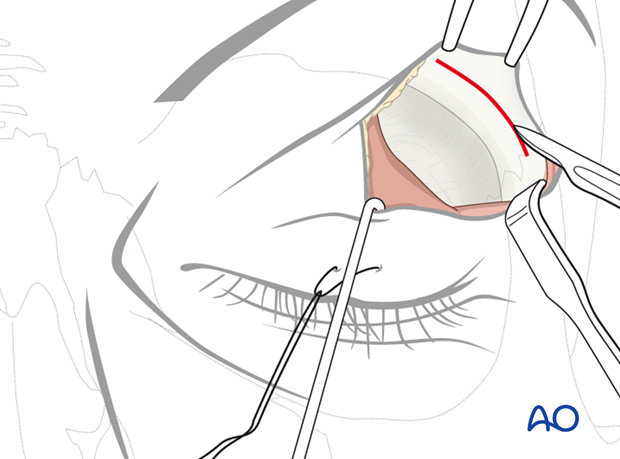
6. Skin incision and undermining of skin muscle flap
The upper-eyelid incision is made using a No. 15 scalpel blade in a medial to lateral direction under digital traction and light pressure of the skin. The skin may be transected together with the orbicularis muscle or each layer separately.
The photograph shows the position of the initial incision through the skin in a supratarsal fold and the underlying orbicularis oculi muscle.
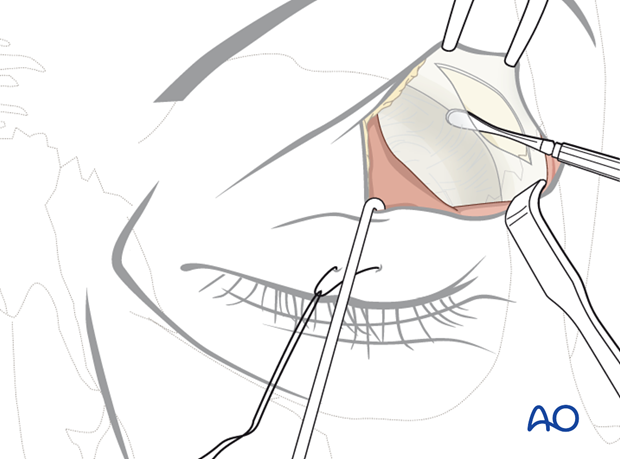
Once the orbicularis muscle is exposed, a small slit is opened at the lateral wound corner to introduce scissors into the preseptal plane and dissection proceeds medially underneath the muscle.
The orbicularis is then divided leaving the orbital septum intact.
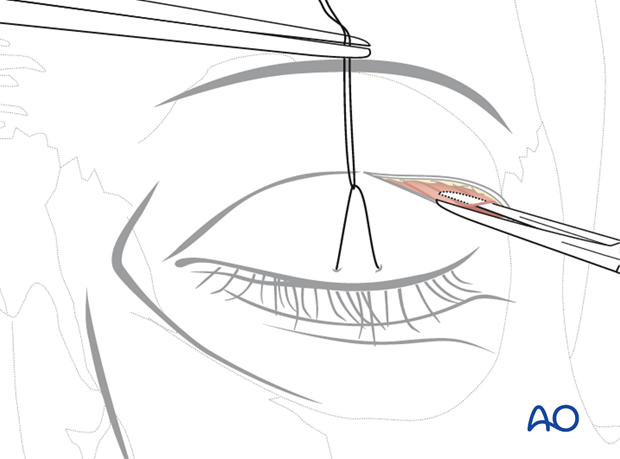
7. Supraperiosteal dissection
The skin muscle flap is also elevated from medial to lateral using scissors. The dissection finally arrives over the superolateral rim with exposure of the periosteum. Commonly in the lateral part of the dissection the retro-orbicularis oculi fat will prolapse.
The vasculature of the muscle provides for skin viability.
8. Periosteal incision
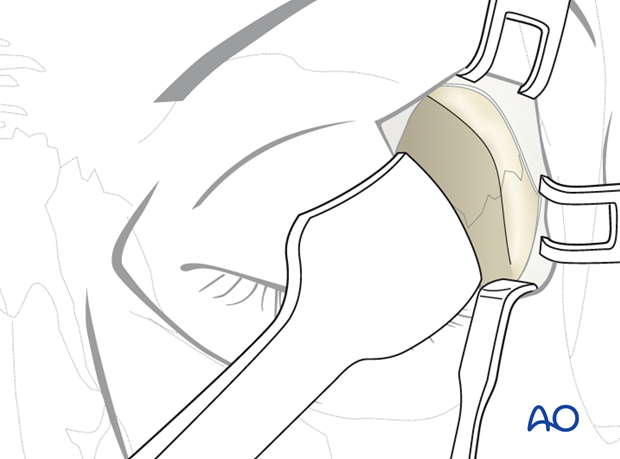
After exposure of its surface, the periosteum is sharply split along the middle of the superolateral orbital rim with a scalpel.
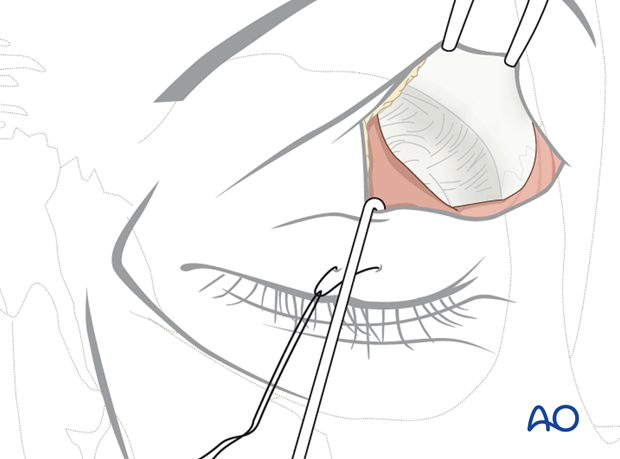
9. Subperiosteal dissection of lateral orbital rim and lateral orbit
The underlying bony structures are exposed using sharp periosteal elevators.
The medial portion of the superolateral orbital rim is first exposed to enter the fossa of the lacrimal gland.
Starting from within this bony concavity inside the anterolateral portion of the orbital roof the periosteal envelope can be reflected from the bony border with sweeping motions of the elevator. When the lacrimal fossa is dissected into the posterior direction the periosteal elevator is oriented into a lateral direction.
The periosteum is then dissected from the lateral and posterior surface of the superolateral rim.
If the periosteum is disrupted, the lacrimal gland may herniate into the surgical field.

In addition to the orbital rim, it is convenient to access the orbital walls inside the superolateral orbital quadrant using the upper eyelid approach.
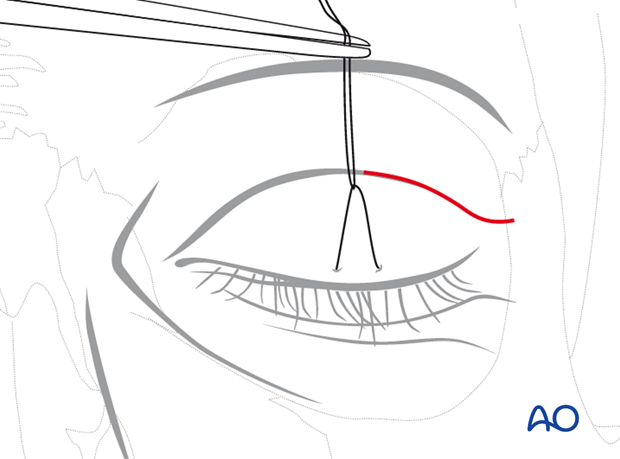
10. Closure
The wound closure is performed in three layers: periosteum, muscle, and skin.
Periosteum
The periosteum is securely closed along the superolateral orbital rim.
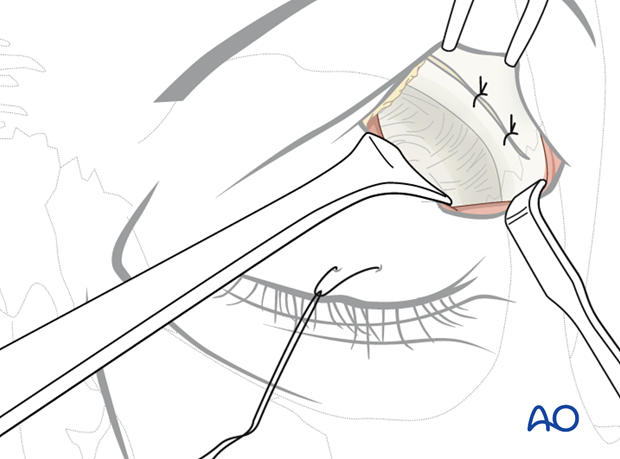
Muscle
The orbicularis oculi muscle is reapproximated with interrupted sutures. The muscle layer is closed meticulously with several interrupted sutures, particularly over the lateral orbital rim. This helps to prevent thinning of the soft tissues covering the bone.
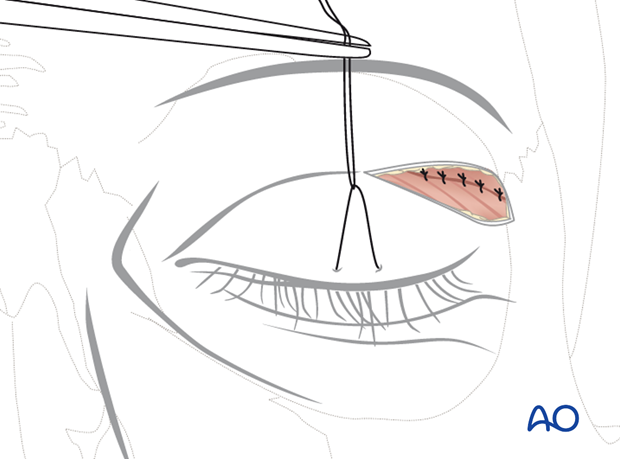
Skin
The final cutaneous closure is made with an interrupted or running suture including the skin edges as well as the underlying orbicularis oculi muscle.