Osteosynthesis in the growing skeleton
Facial fractures in the growing individual are much less common than in adults. While the principles for treating facial fractures (eg, diagnosis, reduction, fixation) are the same, the management of fractures in the growing patient is unique for at least two reasons: developing/unerupted teeth in the maxilla/mandible and growth. Those factors, combined with a young patient's advanced healing potential, may alter the treatment provided compared to what one might do in an adult.
In general, the below points are important considerations when treating young, growing patients.
Greenstick fractures
Many fractures in young patients are incomplete (greenstick) because of bones' elasticity, allowing them to bend rather than break. Such fractures often require no intervention (observation) or reduction with simple manipulation.
Consequences of rapid healing time
Fractures heal very quickly, usually within 3-4 weeks. Therefore, they should be reduced within the first few days, or it may be challenging to do so later. If MMF is used, it can be removed in 3 weeks because most fractures of the maxilla or mandible will have healed in that time. Because of the rapid healing in the young, non-unions are rarely seen.
Maintenance of jaw function
Maintenance of jaw function is imperative because it is essential to allow continued and harmonious growth of the mandible.
If MMF is used, it should only be used for a short time, rarely more than three weeks. If used for more extended periods, especially if there were intracapsular fractures of the mandibular condyle, TMJ ankylosis is possible.

Scarring
Open surgery creates more scarring than caused by the original injury. Scar restricts growth, so the more scar formation, the more the growth will be retarded. For this reason, and in order to avoid injuries to developing dentition, closed techniques are preferred for pediatric cases in comparison to adults with the same injury.
Use of screws
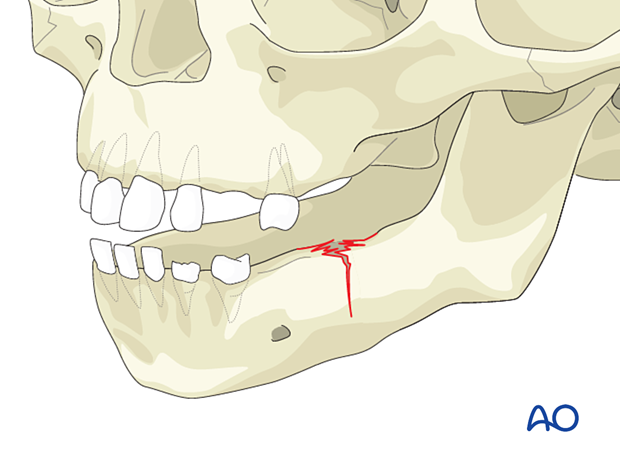
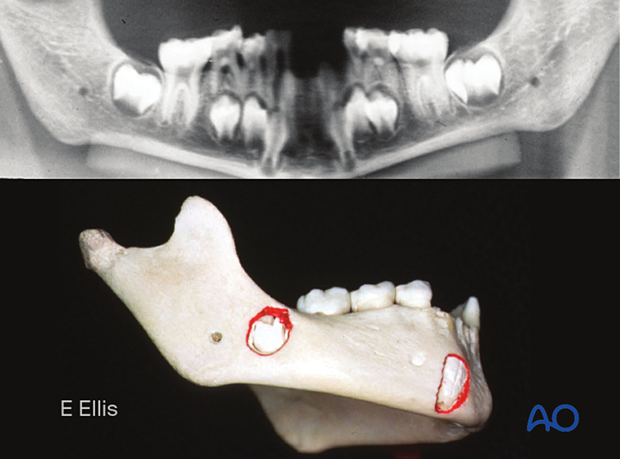
The jaws in the young contain the developing teeth. While open reduction and internal fixation is possible, one must be cognizant of their position and avoid drilling and/or placing screws into them if internal fixation is used.
Soft bone
The bone in the young is soft and may not be of the quality needed for screw retention. Loosening screws with the need for removal may be more common because of the inflammatory response to loose hardware.
Removal of internal fixation devices
Internal fixation devices applied to growing jaws will become internalized (transmigration) secondary to how the jaws grow, with deposition of new bone on the lateral surface and resorption of the lingual surface. If plate removal is desired, it should be performed in less than three months in the actively growing child, or the plate may be challenging to locate and/or remove secondary to being covered by new bone formation. Leaving a plate in place and allowing it to become internalized will not interfere with growth.
Splints
The fabrication and application of acrylic splints secured to the dentition or around the mandible using circummandibular wires can be used to immobilize fractures in the anterior mandible and/or control the width of a multiply-fractured mandible.

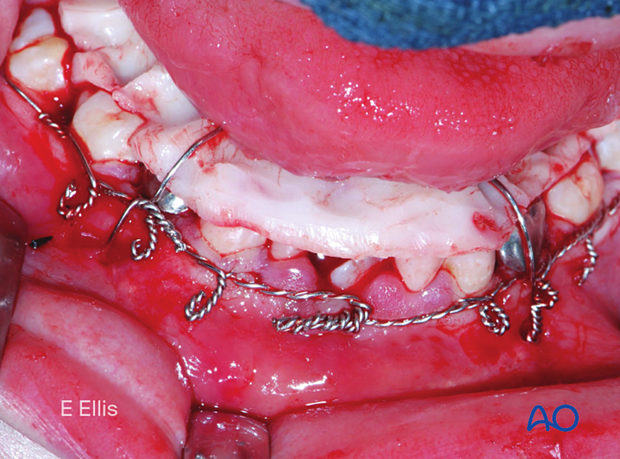
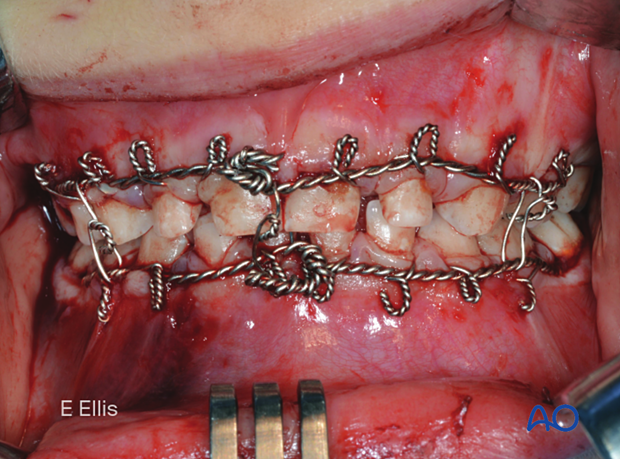
MMF in pediatric patients
The dentition of young patients may be deciduous, mixed, or adult. Because deciduous teeth are short and have minimal heights of contour, placing arch bars is difficult, and the use of Risdon wires is much easier. Patients with mixed dentition may have several missing and/or loose deciduous teeth, making the stable application of tooth-borne appliances (eg, archbars, Risdon wires, etc) difficult. The use of piriform aperture and/or circummandibular wires to maintain the tooth-borne appliances may be required.