Anatomy
1. General considerations
Transoral or transfacial surgical approaches, pin placement for external fixators, reduction, and internal fixation can interfere with the anatomic structures discussed below.
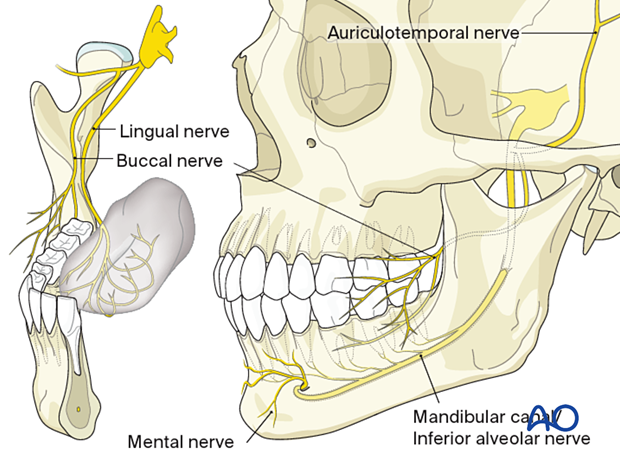
2. Nerves
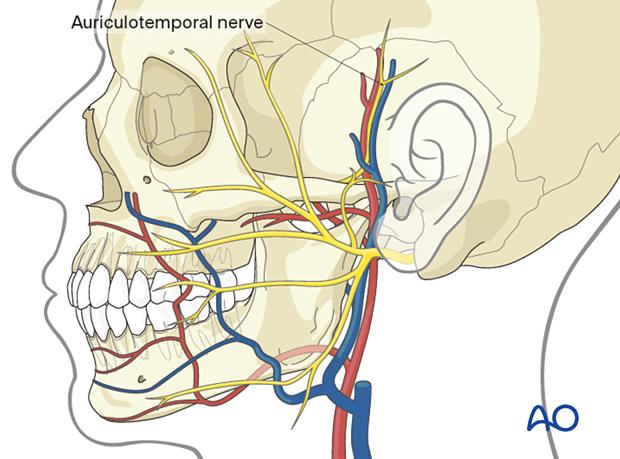
Motor nerve/cranial nerve VII/facial nerve
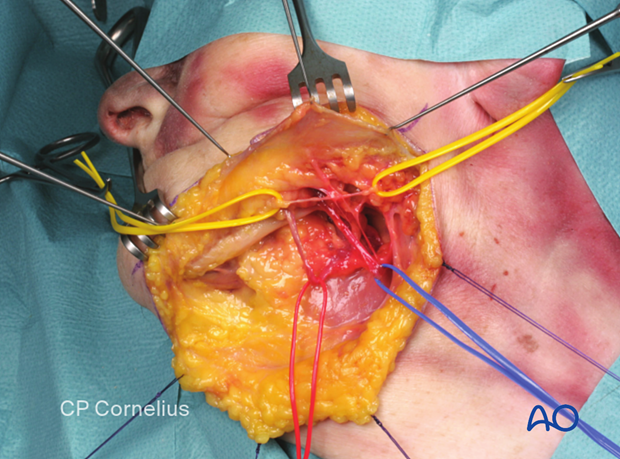
The facial nerve's main trunk and its two major divisions (temporofacial and cervicofacial) cross the mandibular ramus's posterior border in the subcondylar region.
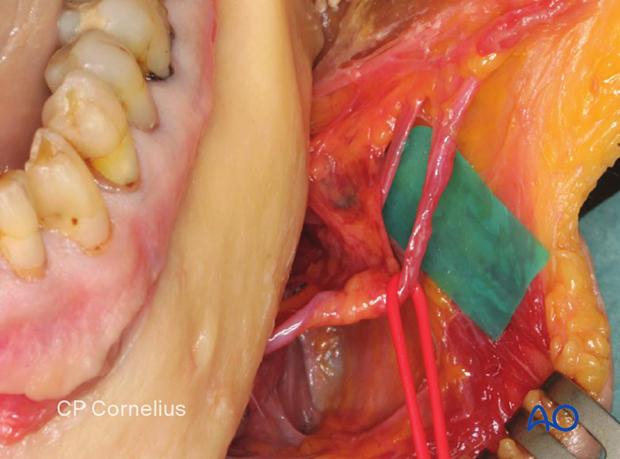
The marginal mandibular branch of the facial nerve is at risk for injury in transfacial approaches to expose the posterior and lateral surfaces of the mandibular ramus (submandibular, retromandibular, facelift approaches).
The facial nerve's frontotemporal branches ascend from the main trunk in a diagonal course to the forehead and are at risk of injury in preauricular or extended coronal approaches.
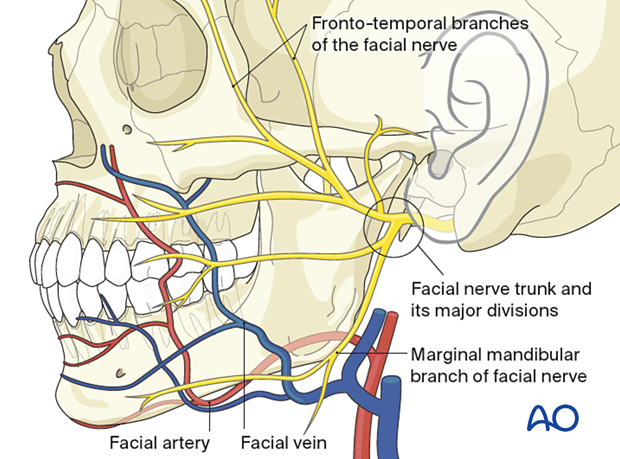
Facial vessels
The facial vessels cross the mandible's inferior border at the level corresponding to the anterior border of the masseter muscle. The vessels are embedded in the lower extensions of the buccal fat pad.
The facial artery is always located anterior to the facial vein. The periosteum separates the facial vessels from the lateral surface of the mandible.
Sensory nerves - branches of the mandibular nerve (CN V3)
Clinically important ramifications of the 3rd division of trigeminal nerve (CN V3)The third or mandibular division of the trigeminal nerve exits the skull base through the foramen ovale into the infratemporal fossa and divides into a smaller mainly motor portion that gives off branches to the muscles of mastication. There is a larger branch that is predominantly sensory in nature. The buccal sensory nerve arises from the smaller portion.
The larger sensory trunk divides into the auriculotemporal, lingual, and inferior alveolar nerves. They provide sensation to:
- parts of the external auditory canal
- the parotid region
- the temporal region
- the inner cheek
- the anterior two-thirds of the tongue
- the floor of the mouth
- the mandibular teeth
- the lower lip/chin area
The auriculotemporal nerve (mainly sensory) loops around the middle meningeal artery by two roots and reunites laterally. Then it curves posteriorly in a plane on the inner aspect of the medial pterygoid muscle and continues superiorly between the temporomandibular joint and the external acoustic meatus before it enters the upper part of the parotid gland and accompanies the superficial temporal vessels. It has several small branches to the temporomandibular joint, to the skin of the external auditory canal and the lateral surface of the tympanic membrane, to the tragus and lower auricular concha, and to supply the facial nerve with sensory and parasympathetic fibers for the innervation of the skin over the parotid region and cheek. The upper terminal branch supplies sensation to the head's lateral side in a zone like the vascularization of the superficial temporal artery.
The auriculotemporal nerve and its branches are at risk for injury in external preauricular approaches to the temporomandibular joint, extended coronal approaches, and rhytidectomy incisions.
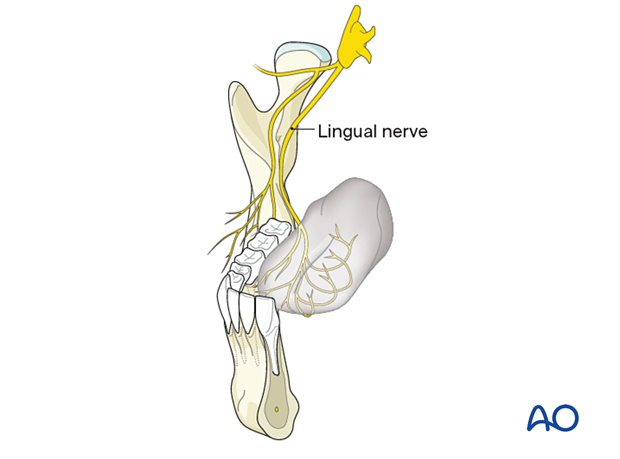
The lingual nerve lies anterior to the inferior alveolar nerve and first descends deep to the lateral pterygoid muscle and superficial to the medial pterygoid muscle. From the lower border of the lateral pterygoid muscle, the nerve passes obliquely forward between the medial pterygoid muscle and the ascending ramus's inner aspect until it reaches the bottom fold of the pterygomandibular space. At the posterior mylohyoid line-height, it exits the space and curves anteriorly to take a longitudinal direction. For a short distance, it lies close to the lingual cortex of the inner mandibular angle (temporal crest), the retromolar trigone, and the third molar region. Towards the oral cavity, it is covered by the mucous membrane and the posterior tail of the submandibular gland so that it can often be visualized as a pale shade by tightening the soft tissues of the posterior glossoalveolar sulcus. On its course to the dorsum and the tongue's tip, it turns medially and crosses the lateral side of the superior pharyngeal constrictor, styloglossus, and hyoglossus muscles to split into its terminal branches.
Exiting from the petrotympanic fissure, the chorda tympani joins the lingual nerve's back at an acute angle at the lateral pterygoid muscle level.
The lingual nerve provides pain, temperature, and touch sensation to the anterior two-thirds of the tongue, the glossoalveolar sulcus, and the lingual gingiva of the entire lower quadrant. Taste mediating fibers from the anterior two-thirds of the tongue are conveyed centrally via the chorda tympani. The chorda tympani also contains visceral efferent fibers traveling to the sublingual and submandibular glands.
The lingual nerve is prone to injury during intraoral approaches exposing the medial side of the retromolar trigone and the ascending ramus's inner aspect. Sometimes the nerve is damaged during drilling or transverse screw insertion along the upper border (oblique line) of the inner bony angle. The chorda tympani itself is out of reach during fracture repair procedures, but its fascicles inside the lingual nerve can be affected.
The inferior alveolar nerve (IAN) is the largest branch of the mandibular nerve and carries sensory and motor fibers. On its way from the infratemporal fossa and mandibular foramen at the medial surface of the ascending ramus, it descends in a parallel route (posterior and lateral) to the lingual nerve. The mylohyoid nerve branches off posteriorly just before the main nerve enters the mandibular foramen. The mylohyoid nerve runs inferiorly and anteriorly in the mylohyoid groove and further forward into the digastric triangle. It provides motor innervation to the mylohyoid muscle and the anterior belly of the digastric muscle. It provides sensory fibers that supply a small circular zone of skin above the mental protuberance.
Furthermore, the IAN can separate collateral branches in its precanalicular segment, which independently run downward on the bony surface and pierce into the bone through accessory foramina and small vents in the retromolar area. If encountered during exposure at the inner angle, it is hard to decide whether they can be transected because their contribution to the sensory innervation is never known.
The IAN is accompanied by the inferior alveolar vessels in its course through the mandibular canal.
The mandibular canal can be positioned at a variable vertical height that has to be assessed in the preoperative imaging. The IAN's fascicles can either unite into single or double-stranded bundles and ramify into an ample plexus formation within the canal or their intraosseous course. These neural structures give rise to the inferior dental branches and the inferior gingival branches, providing sensation to the teeth and gums. The latter branches often do not directly stem from the inferior alveolar nerve bundle or plexus but arise as a second series from the dental branches.
The IAN bifurcates at the mental foramen with a major portion exiting as the mental nerve to the lateral side. The minor quantity of fibers continues anteriorly inside a canalicular structure as an incisal bundle.
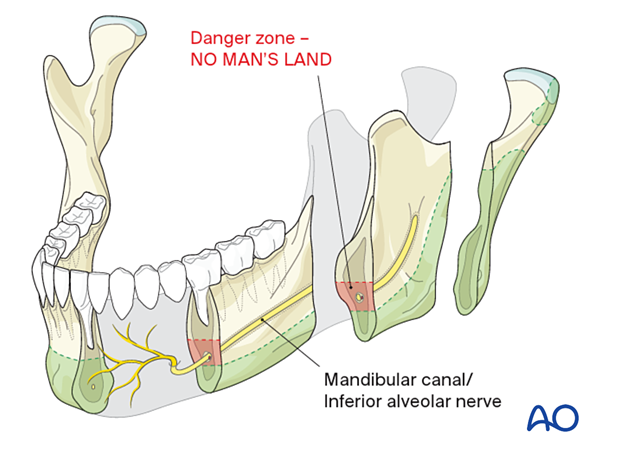
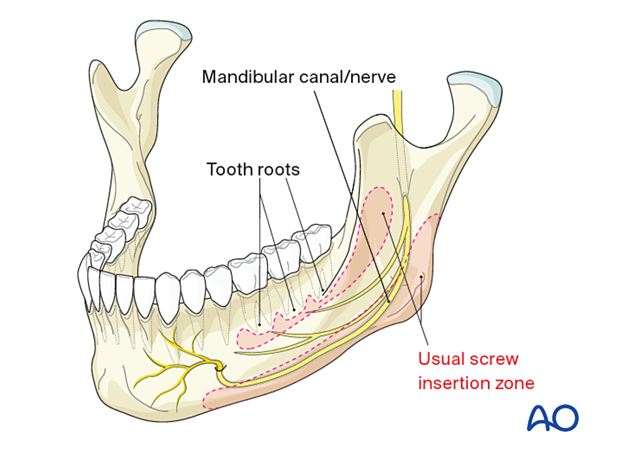
As a matter of principle, the intraosseous IAN structures are at potential risk for injury by drilling and inserting osteosynthesis screws and must be located on preoperative radiographs.
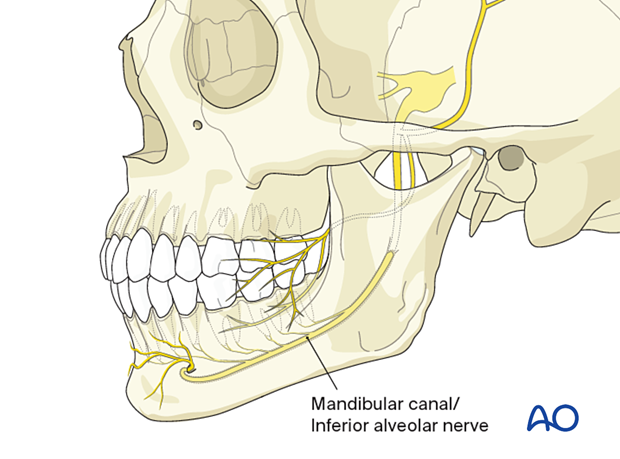
There may be variations of the course of the mandibular canal and the inferior alveolar nerve. The typical situation is depicted in the previous step, but the canal's vertical height can be located next to the mandible's lower border (as illustrated here).
The alveolar nerve itself can consist of a single bundle inside the canal, but it can also spread in a plexus formation inside the overall bony cross-section of the mandible. These situations prevent the usual screw insertion and require an individualization of screw and/or plate placement.
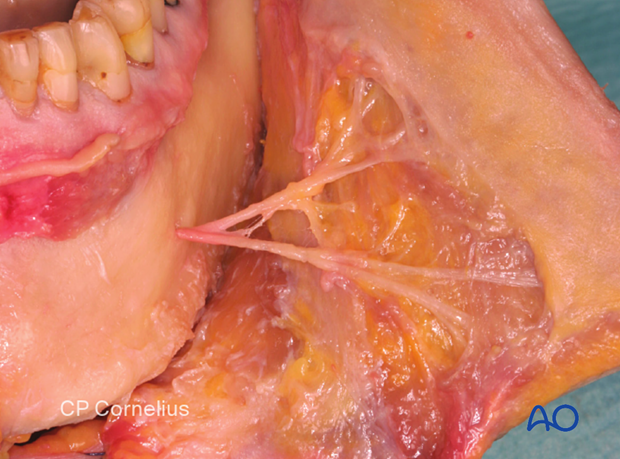
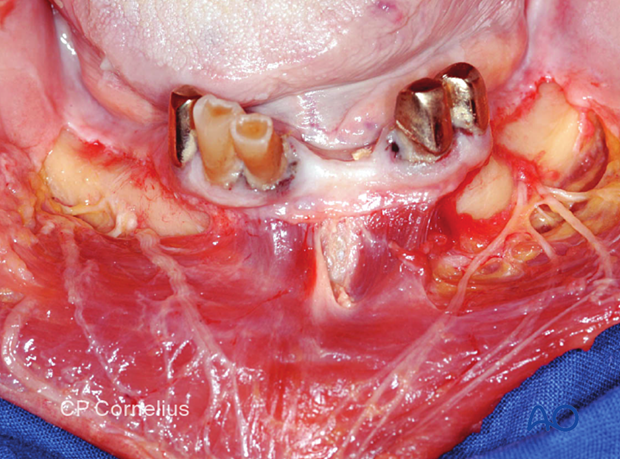
Mental nerve (mental neurovascular bundle)
The mental neurovascular bundle exits the mental foramen, which is the anterior opening of the mandibular canal. The bony foramen is usually positioned at a vertical height midway between the mandibular body's alveolar and basal border just below the premolars' apices. In the sagittal plane, the mental foramen is located between the first and second premolar root tips.
The mental nerve is the major terminal branch of the inferior alveolar nerve. The branches enter the chin's skin, the vestibular gingiva in the symphyseal region, and the labial sulcus's mucosa, and the lower lip vermillion.
Photographs show the branches of the mental nerve.
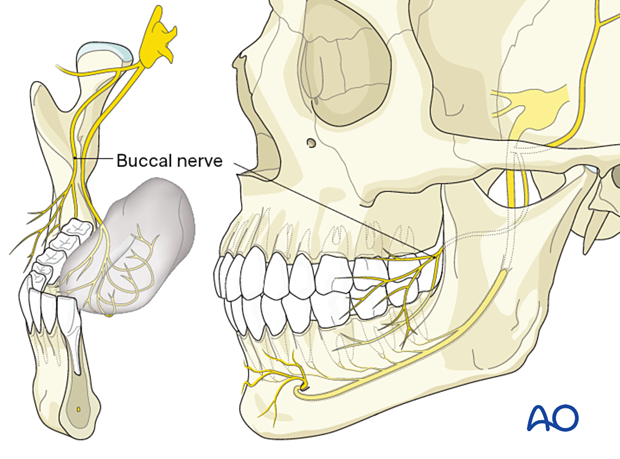
Buccal nerve
The buccal nerve (sensory branch of the mandibular nerve) passes medial to the ascending ramus and divides into many small branches overlying the buccinator muscle's lateral surface. The terminal branches pierce the muscle for the buccal gingiva's innervation up to the premolar area and the buccal mucosa between the pterygomandibular raphe and the corner of the mouth.
3. Muscles
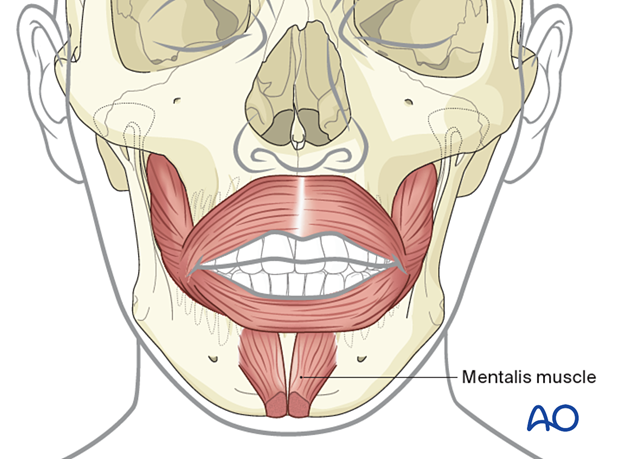
Mentalis muscle
The mentalis muscles are paired and function as elevators of the lip and chin. They arise directly from the anterior symphysis's bony surface in a zone between the labial sulcus and the lower incisors' apices, located in front of the mental foramina. If the mentalis muscle is cut during an anterior vestibular approach, it must be carefully reattached to avoid a sagging or drooping chin.
Buccinator muscle
The buccinator muscle's bony attachments run a course below the mucogingival junction opposite to the molars and along the oblique line ascending as the anterolateral rim of the ascending ramus. The attachments extend back into the pterygomandibular raphe. The buccinator is innervated by the buccal branch of the facial nerve. The muscle belongs to the mimetic muscle system and has a unique functional structure allowing for movement comparable to peristaltic motion. Its detachment can result in an impaired bolus transport.
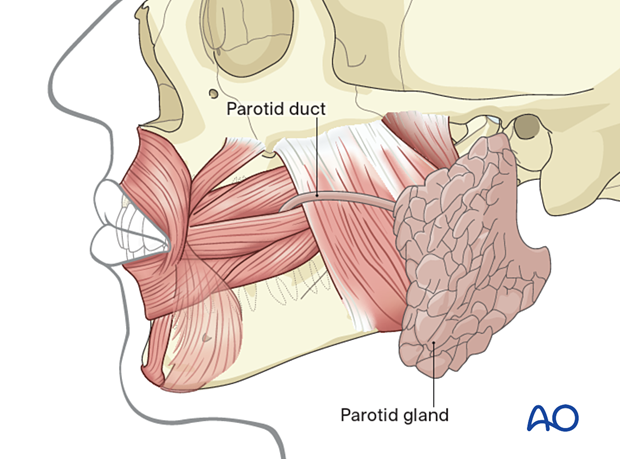
The duct of the parotid gland pierces the buccinator muscle and exit besides the superior molar area.
Reminder: The buccinator muscle belongs to the mimetic muscle system and has a unique functional structure allowing for a movement comparable to a peristaltic motion. The deep fibers run in parallel bundles from the modiolus to the pterygomandibular raphe at the occlusal plane's level and account for the buccinator mechanism building up a ridge towards the occlusal plane. Its detachment can result in an impaired bolus transport out of the buccal space, which can be annoying for the patient. The buccinator is innervated by the buccal motor branch of the facial nerve.
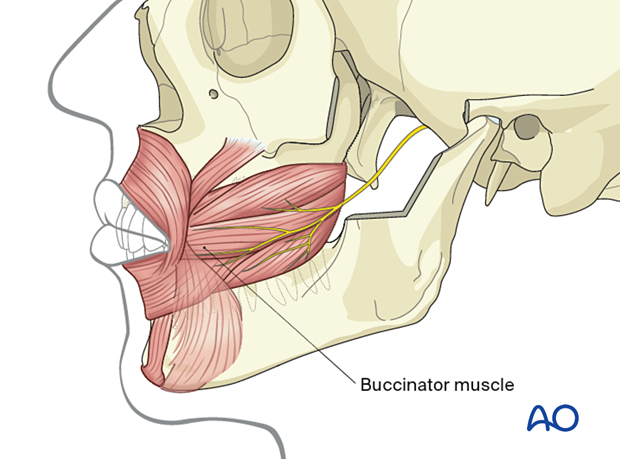
The duct of the parotid gland pierces the buccinator muscle and exits besides the superior molar area.
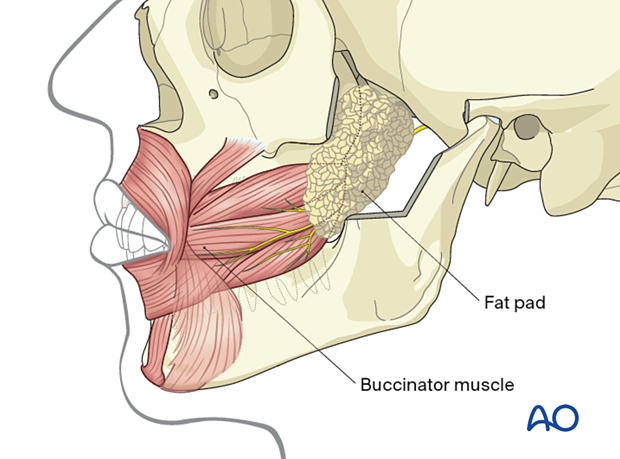
Buccal fat pad
The buccal fat pad is located in an extended three-dimensional compartment with its main mass or cheek portion overlying the buccinator muscle's posterolateral aspect and the maxillary tuberosity, which is partly covered by the anterior border of the masseter muscle. The major processes of the fat pad stretch into the deep temporal, pterygomaxillary and pterygoid region. The fat is distinct from facial fat and like orbital fat in consistency and globule-like structure, to which it connects through the infraorbital fissure. The facial vessels run along the anterior border of the cheek portion. The fascial layers (capsule) enveloping the buccal fat pad on the medial surface next to the buccinator muscle are rarely ruptured in a subperiosteal dissection along the mandibular body and angle. However, when going up the ramus after a vertical division of the buccinator muscle anterior to the pterygomandibular raphe to reach beyond the coronoid notch, the inner capsule of the fat pad can be breached, leading to a herniation that will obstruct the vision in the surgical field.
4. Bony cross sections and intraosseous structures
Intraosseous structures to be avoided when operating on the mandible are:
- Tooth roots
- Mandibular canal/inferior alveolar nerve/no man's land
See also:
Heibel H, Alt KW, Wächter R, Bähr W (2001) Cortical thickness of the mandible with special reference to miniplate osteosynthesis. Morphometric analysis of autopsy material
Mund Kiefer Gesichtschir; 5(3):180-5.