Transoral approach to the condylar process and ramus
1. Principles
Vestibular incisions
The extended vestibular incision can be used for standard fracture fixation techniques or in conjunction with endoscopically assisted surgical techniques.
The ramus and condyle region can be exposed via a transoral approach by extending the standard vestibular incision in a superior direction up the ascending ramus.
The incision can be altered depending on the area of the ramus/condylar process that needs exposure and treatment.
Oral contamination is not a contraindication for an intraoral incision.
In complex fractures, including comminuted and avulsive fractures that require the placement of load-bearing reconstruction plates, a transfacial/transcutaneous approach can provide better access to treat the injury.
2. Anatomical considerations
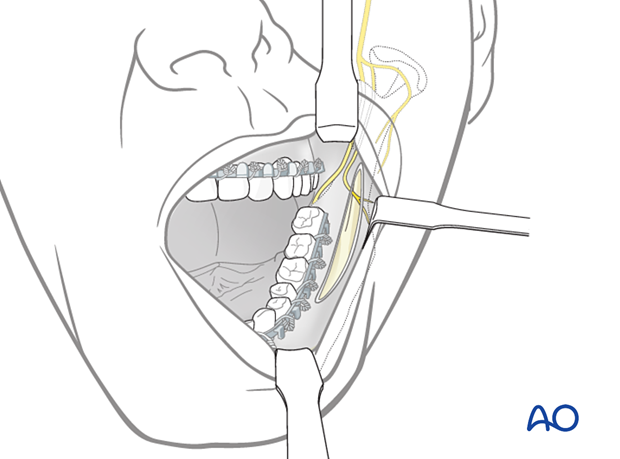
Sensory buccal nerve
The sensory buccal nerve crosses the upper anterior rim of the mandibular ascending ramus in the coronoid notch region. It is usually below the mucosa running above the temporalis muscle fibers. When the posterior vestibular incision is carried sharply along the bony rim, the buccal nerve is at risk of transsection resulting in numbness in the buccal mucosal region. Therefore, to protect the nerve, the posterior incision is extended bluntly as soon as the lower coronoid notch is reached.
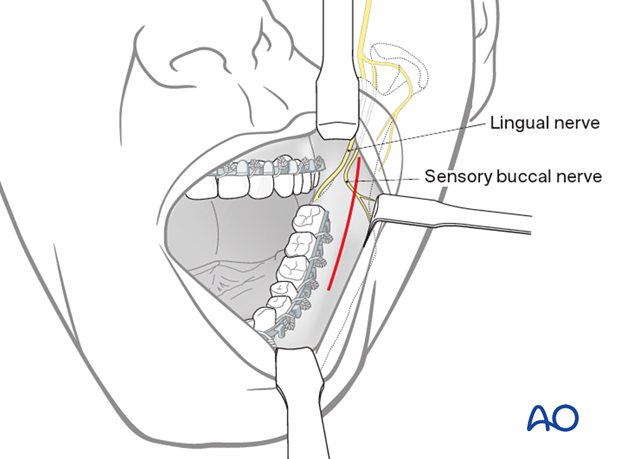
This photograph shows the buccal sensory nerve.
Buccinator muscle
The lateral mucogingival vestibular incision transects the lower attachment of the buccinator muscle. Lateral stripping of the mucoperiosteal flap disrupts the attachment of the muscle. To reattach the muscle, the sutures for wound closure in the lateral vestibular should not only be superficial. The suture should catch all layers (mucosa and muscle) as a safeguard for muscle reattachment.
The buccinator muscle belongs to the mimetic muscle system and has a unique functional structure allowing for a movement comparable to a peristaltic motion. The deep fibers run in parallel bundles from the modiolus to the pterygomandibular raphe at the occlusal plane's level. They account for the buccinator mechanism building up a ridge towards the occlusal plane. Its detachment can result in an impaired bolus transport out of the buccal space, which is troublesome for the patient. The buccinator is innervated by the buccal motor branch of the facial nerve.

3. Vestibular incision
Unless contraindicated, infiltrate the area with a local anesthetic containing a vasoconstrictor.
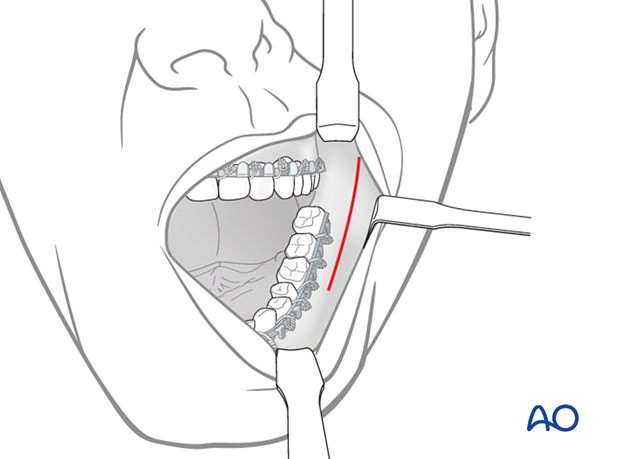
Make an incision through the mucosa in the vestibule approximately 5 mm away from the attached gingiva (in the mucogingival junction), extending up the external oblique ridge.
4. Exposure of fracture
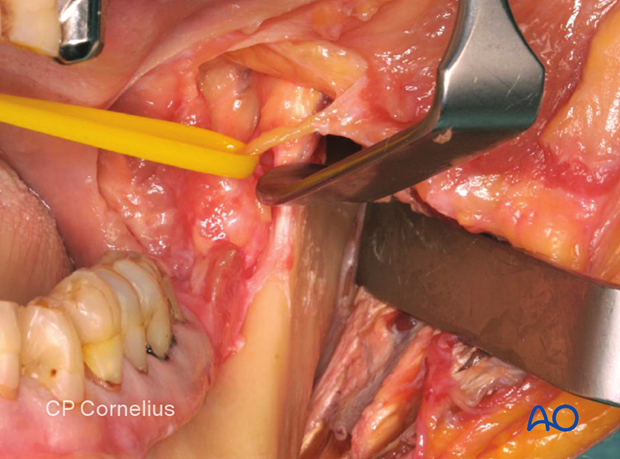
The ramus and condylar process's lateral surface is exposed in a subperiosteal plane to visualize the fracture. Right-angled retractors and fiberoptic lighting facilitate this procedure.
The surgeon can treat the fracture through the transoral approach under direct vision or opt for endoscopic assistance.
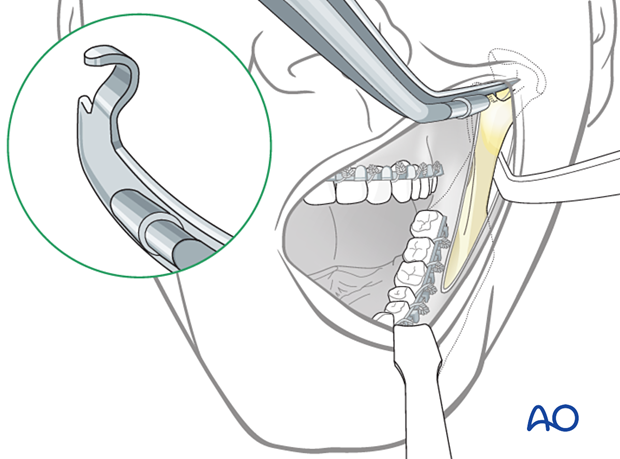
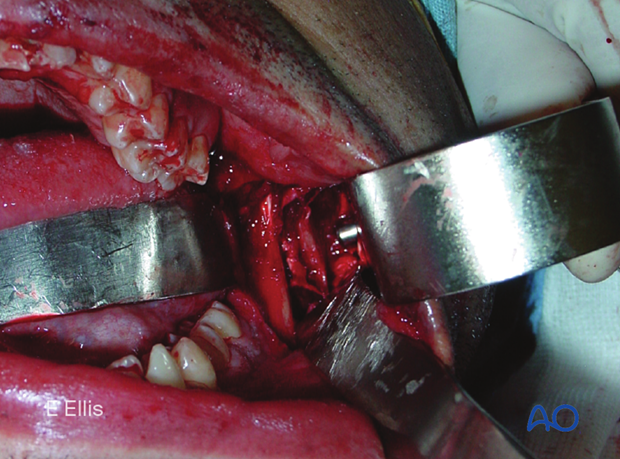
Fixation can be applied either transbuccaly or with right-angled instrumentation.
This image shows a clinical example of transbuccal trocar instrumentation.
5. Wound closure
After thoroughly irrigating the wound and checking for hemostasis, the incision is closed using interrupted or running resorbable sutures.
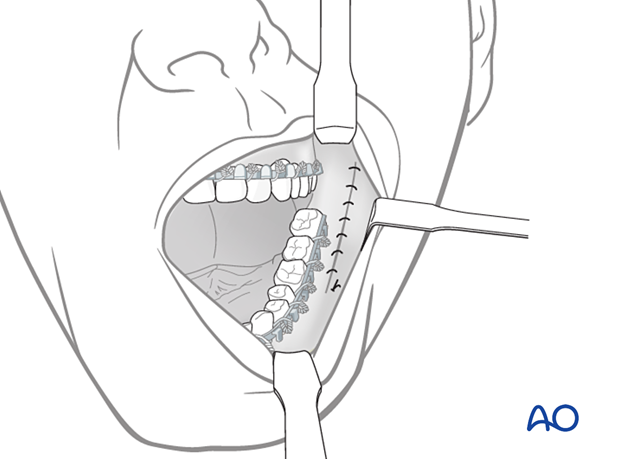
An elastic pressure dressing covering the ramus/condylar process region helps support the soft tissues and prevent hematoma formation.