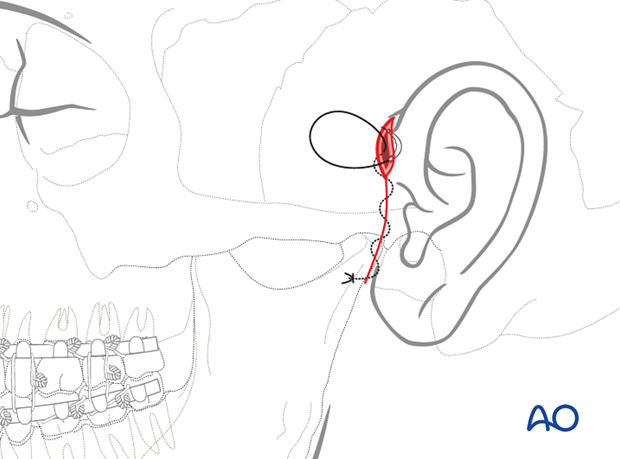
Preauricular approach
1. Principles
General considerations
The preauricular approach gives access to fractures in the mandibular condylar head and neck region. Many surgeons who perform temporomandibular joint (TMJ) surgery routinely use this incision to access the temporomandibular joint.
The illustration demonstrates the access and the amount of exposure.
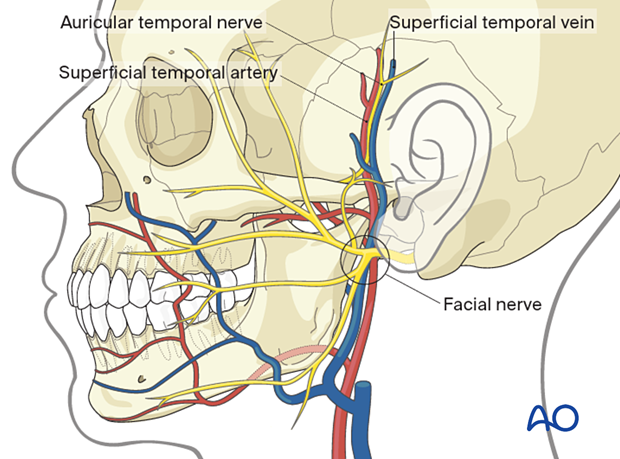
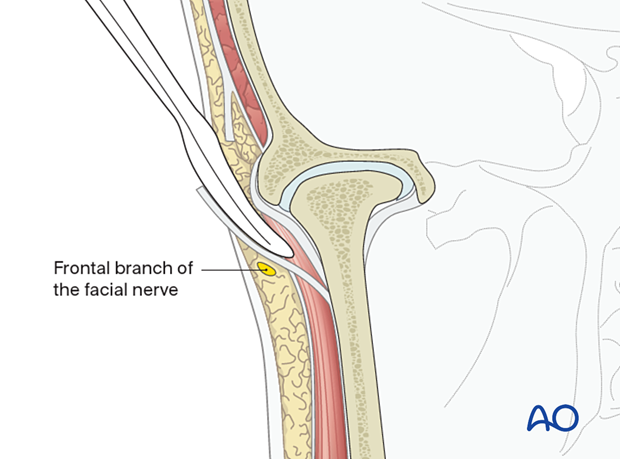
Neurovascular structures
Branches of the facial nerve may be involved in this incision and dissection.
The superficial temporal artery and vein are commonly encountered in this surgical approach. The vessels should be conserved if possible.
Exposure
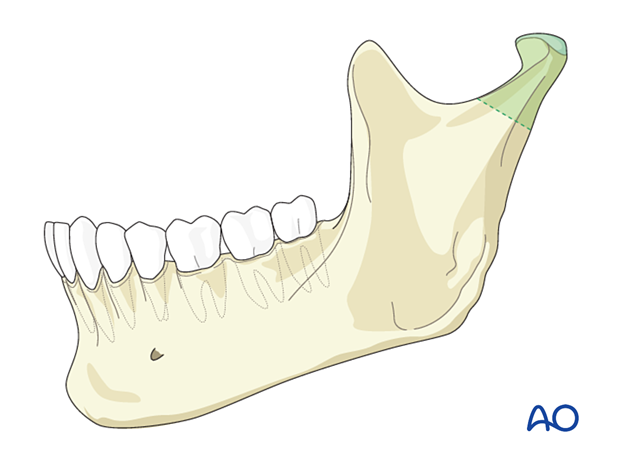
The exposure offered by the preauricular approach is limited.
Only a limited portion of the condylar neck region can be reached.
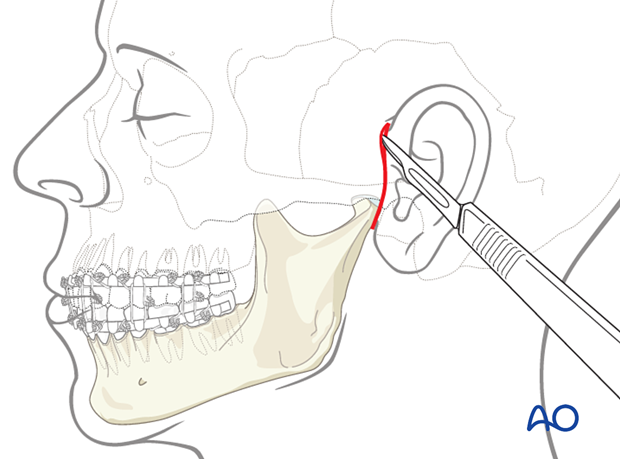
2. Skin incision
General consideration
The use of a solution containing vasoconstrictors ensures hemostasis at the surgical site. The two options currently available are the use of local anesthetic or a physiologic solution with vasoconstrictor alone.
Use of a local anesthetic with vasoconstrictor may impair the facial nerve's function and impede the use of a nerve stimulator during the surgical procedure. Therefore, consideration should be given to using a physiological solution with vasoconstrictor alone or injecting the local anesthetic with vasoconstrictor very superficially.
Muscle relaxants used in general anaesthesia can also impair nerve function and must be avoided.
Make the incision in a preauricular skin crease from the level of the helix above the tragus to the level of the lobule .
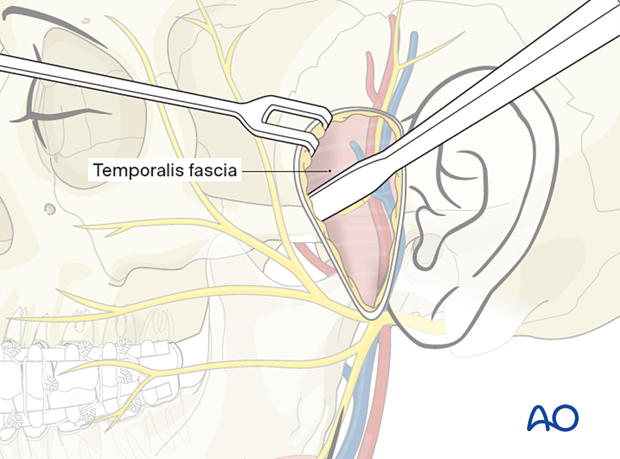
3. Dissection
Locating temporalis fascia
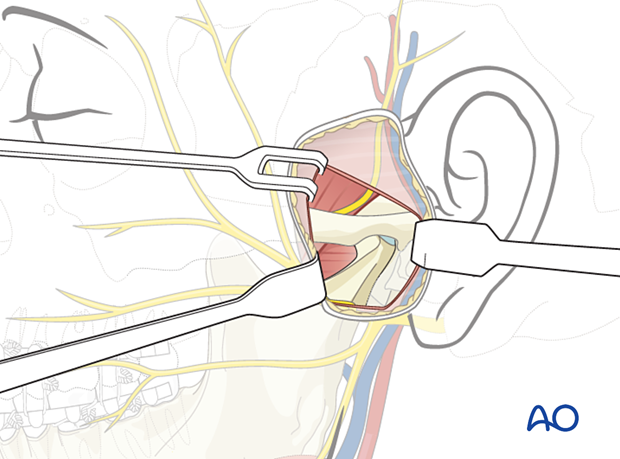
Carry the incision through the skin and subcutaneous tissues to the depth of the temporalis fascia. The temporalis fascia is a glistening white tissue layer that is best appreciated in the incision's superior portion.
The superficial temporal vessels may be retracted anteriorly with the skin flap (sectioning some posterior and superior branches) or left in place.
The zygomatic arch can easily be palpated at this point of the dissection. The lateral pole of the mandibular condyle can also be palpated. Palpation can be facilitated by having a surgical assistant to manipulate the jaw.
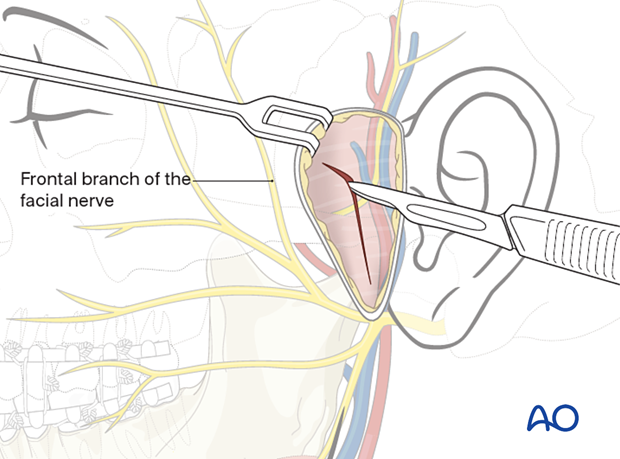
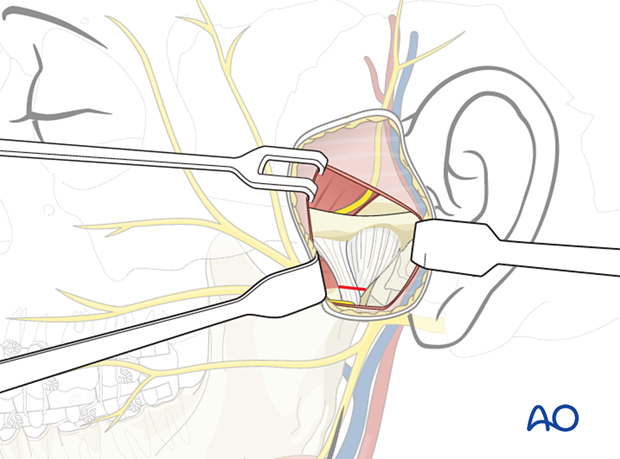
Incising temporalis fascia
Make an oblique incision parallel to the course of the facial nerve's frontal branch, through the superficial layer of the temporalis fascia above the zygomatic arch.
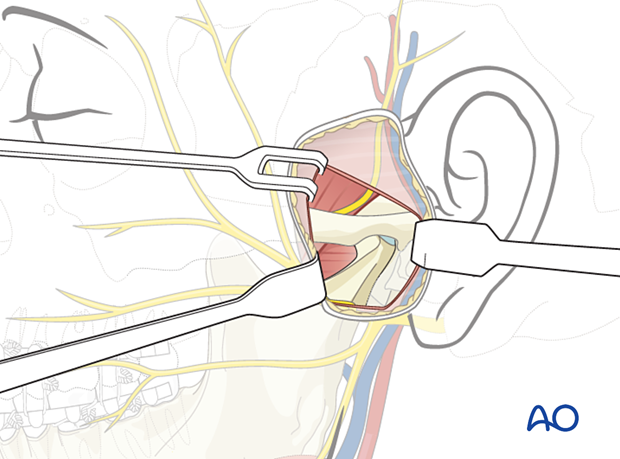
Dissection of the joint capsule
Insert the periosteal elevator beneath the temporalis fascia's superficial layer and strip the periosteum off the lateral zygomatic arch.
Dissection will be carried inferiorly to expose the capsule of the TMJ.
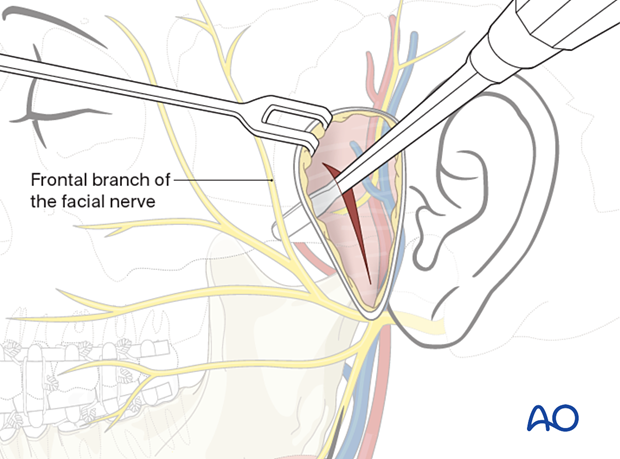
This illustration shows the coronal view of dissection to the lateral portion of the zygomatic arch and mandibular condyle region.
4. Optional: capsule incision
In the rare case of treating condylar head fractures, the TMJ capsule is horizontally incised at the level where the capsule meets the condylar neck.
Dissection can be carried inferiorly in a subperiosteal plane to reach the neck of the mandibular condyle.
5. Wound closure
If the TMJ capsule has been incised to access the condylar head, it must be closed as the first step.
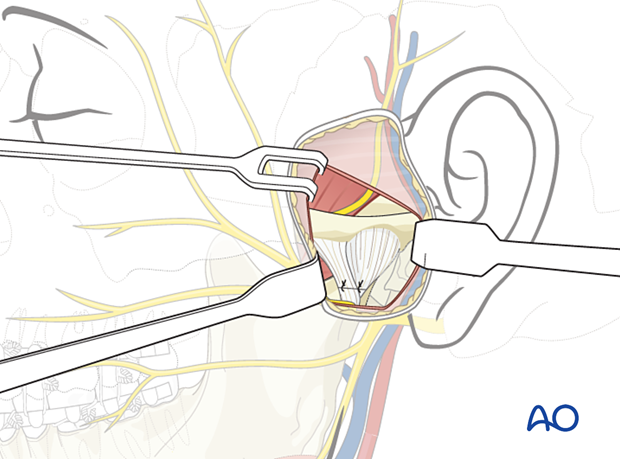
The temporalis fascia is closed as the next step.
Skin and subcutaneous sutures are placed.
A pressure dressing and/or drain may be used according to the surgeon's preference.