Repositioning and fixation
1. Decision/Indication
Tooth intrusion is associated with a potential risk of loss of the affected tooth due to replacement resorption (ankylosis) or infection related resorption. Treatment methods are only partly evidence based. Prognosis in all cases is uncertain.
Surgical repositioning and fixation
This treatment technique is preferable in the acute phase and in permanent teeth. Intrusion with major dislocation of the tooth (approximately more than half a crown length) may indicate surgical repositioning.
Orthodontic repositioning
This treatment may be preferred for patients coming in for delayed treatment and enables repair of marginal bone in the socket along with the repositioning of the tooth.
Await spontaneous eruption
This is the treatment of choice for deciduous/primary teeth and for teeth with incomplete root formation.
Common for all treatments
Endodontic treatment is to prevent the necrotic pulp initiating infection-related root resorption. This treatment should be considered in all cases with completed root formation where the chance of pulp revascularization is very minimal. Endodontic therapy should preferably be initiated within 3–4 weeks posttrauma.
2. Surgical repositioning and fixation
Principles
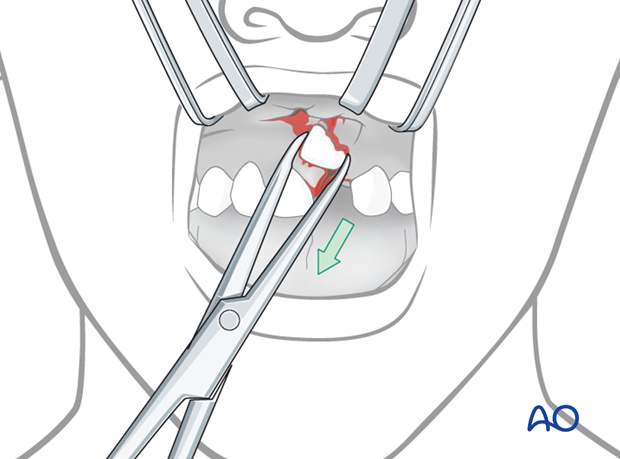
Under local or general anesthesia, the tooth may be guided to it’s proper position by means of an extraction forceps, and soft-tissue repair may precede the fixation of the tooth. The tooth should be fixed after repositioning with acid etch/resin technique in a manner that will promote healing of the periodontal ligament, ie, no hard contact between tooth and bony socket.
Arch bar fixation is not recommended, since it implies displacement during tightening of steel wires which further adds to the risk of trauma to the periodontal ligament, with subsequent replacement resorption of the root.
Sequence of procedure
- Local or general anesthesia
- Surgical repositioning of the tooth
- Soft-tissue repair (if necessary)
- Fixation of tooth
- Aftercare and follow-up
Tetanus
If the injury occurred outdoors and the wound is contaminated with soil, tetanus prophylaxis should be considered.
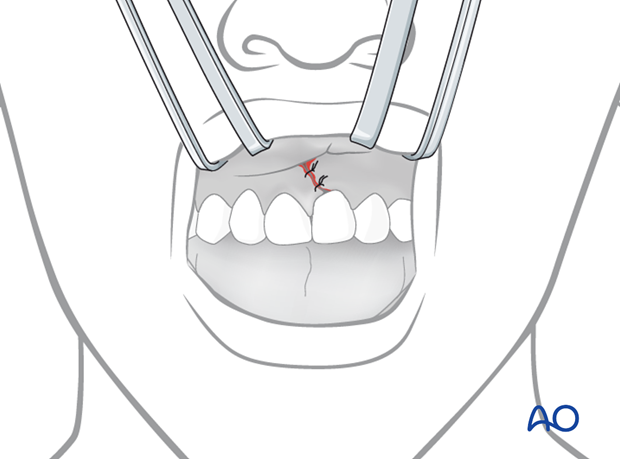
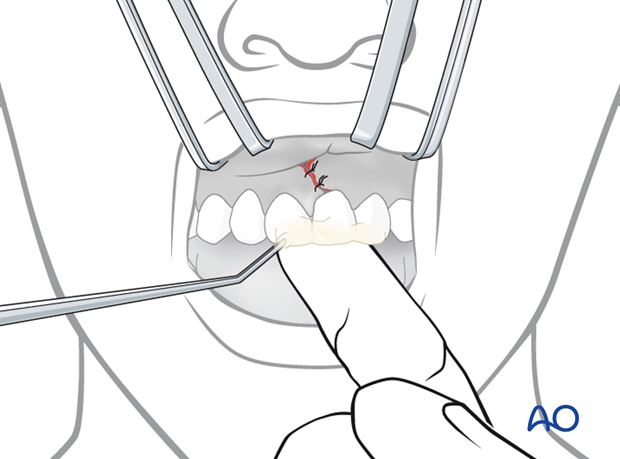
Repositioning
Repositioning becomes increasingly difficult with increasing depth of intrusion of the tooth. In most cases a gingival laceration is present which provides sufficient access to the tooth.
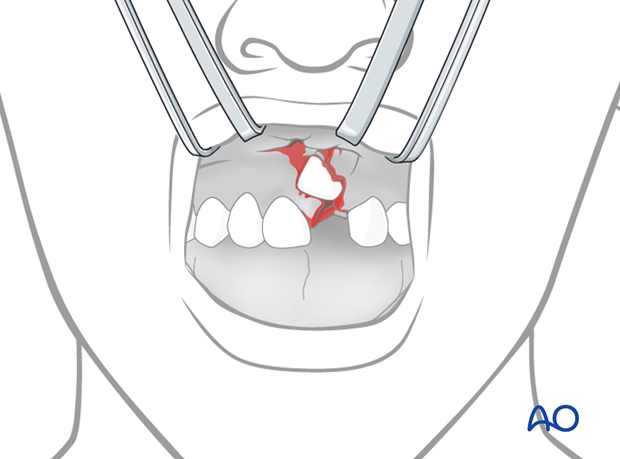
The tooth is pulled by the forceps and placed in its proper position.
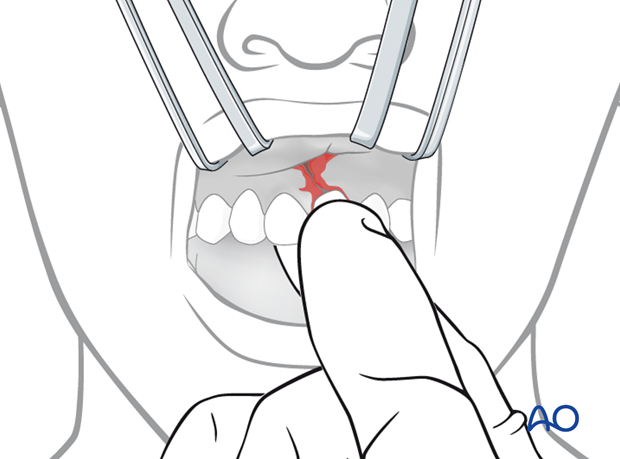
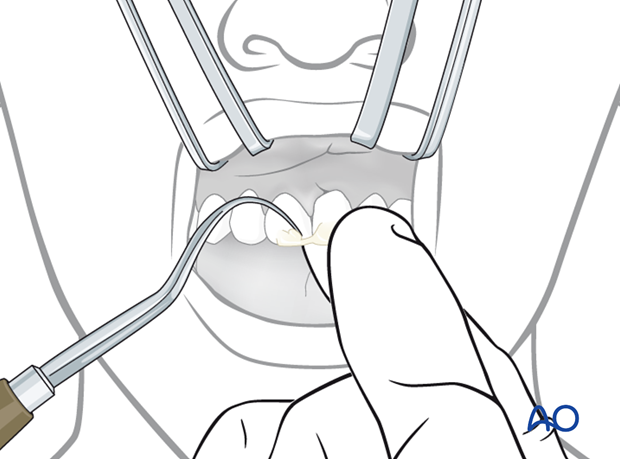
When the tooth is in position, the neighboring displaced bone may be molded to its proper position by digital pressure to promote healing.
In case of gross comminution of the alveolar bone and lacerations of soft tissues, the tooth may temporarily be placed in saline solution while remodeling the osseous tissues and repair the soft tissues by means of suturing.
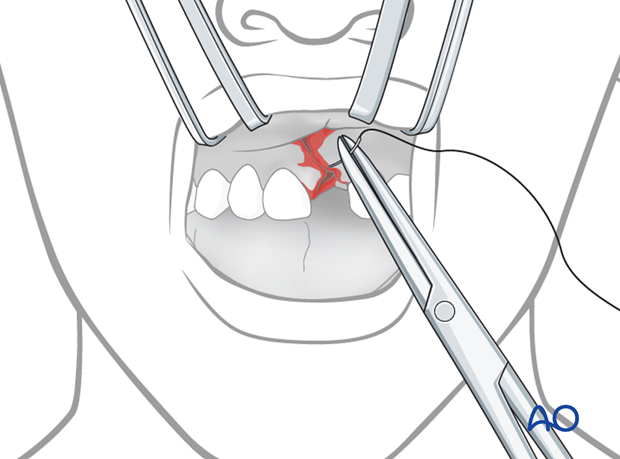
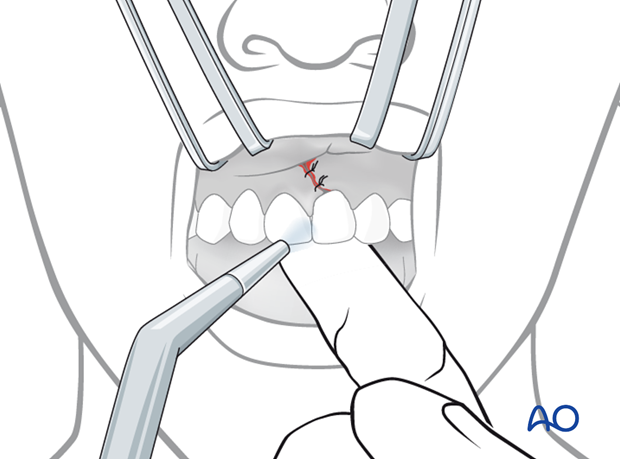
Soft-tissue repair
The wound should be rinsed with saline solution if contaminated with foreign bodies. Repair of tears should be completed before working with the acid etch/resin technique. Drying of the tooth with compressed air or absolute alcohol should be avoided in the presence of open wounds.
Monophilic nylon is preferred as a suture material in case of lacerated gingiva or mucosa. Interrupted sutures are the standard of care of wound closure in lacerated gingival wounds.
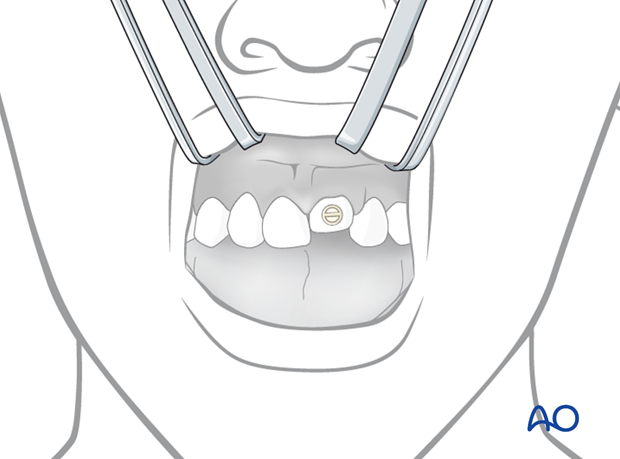
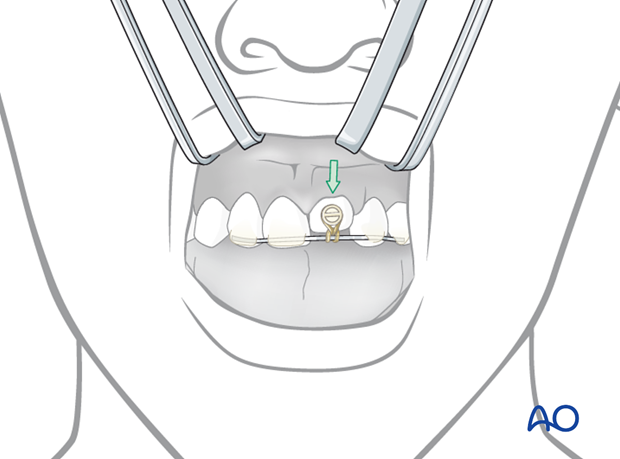
Fixation
Fixation is preferably accomplished with acid etch of the incisal enamel and application of a resin splint involving intact neighboring teeth. The teeth involved are gently dried with compressed air (as illustrated) or absolute alcohol and kept dry during the fixation procedure.
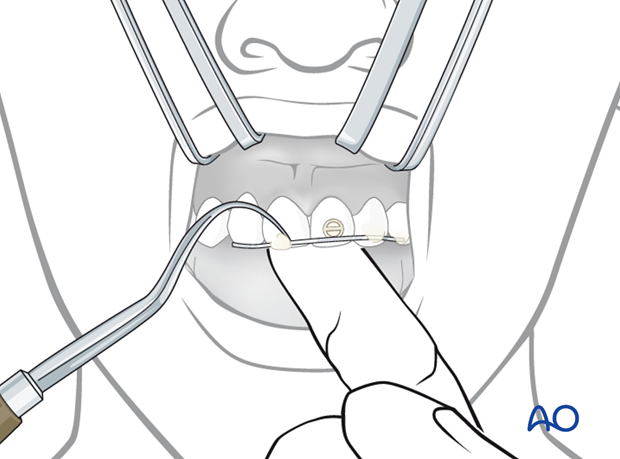
A finger on the lingual aspect of the tooth can maintain tooth position during the fixation procedure.
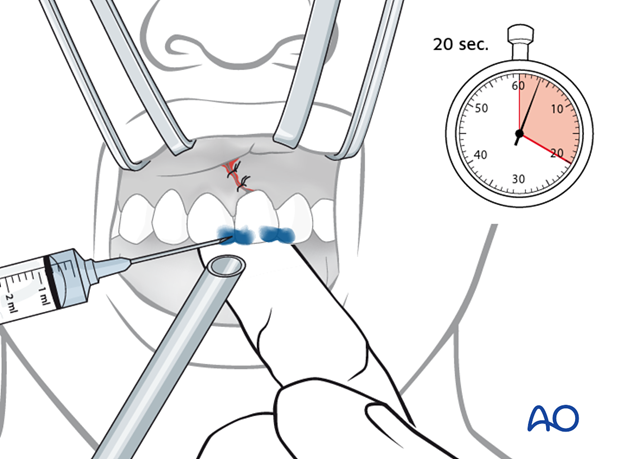
Points of fixation in the repositioned tooth as well as neighboring teeth are etched with phosphoric acid for 20 seconds.
Remember to place a suction tube to maintain dryness during etching procedure.
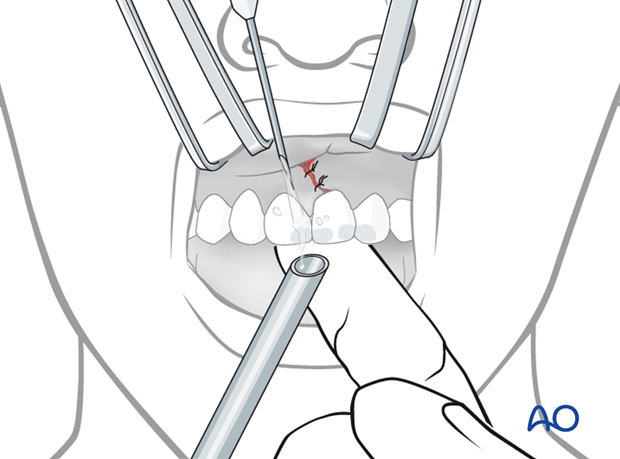
The etch gel is removed by saline irrigation. Make sure to direct the saline jet in a direction away from soft-tissue wounds and to place a suction tube to remove the spray of the saline and etch gel.
The fixation spots are then dried.
It is imperative that the enamel be kept dry until the resin has completely set.
Resin material (eg, as used for temporary crowns and bridges) is applied to provide a splint. This material allows a certain flexibility of splinting and is easy to remove.
Fixation should generally be maintained for 4 weeks in the case of intrusion in order to allow healing of crushed or fractured bone.
Note: the patient should be put on soft diet for 2 weeks. Exposure to temperature extremes should be avoided.
Note: care has to be taken that there is no occlusal loading to the affected tooth.
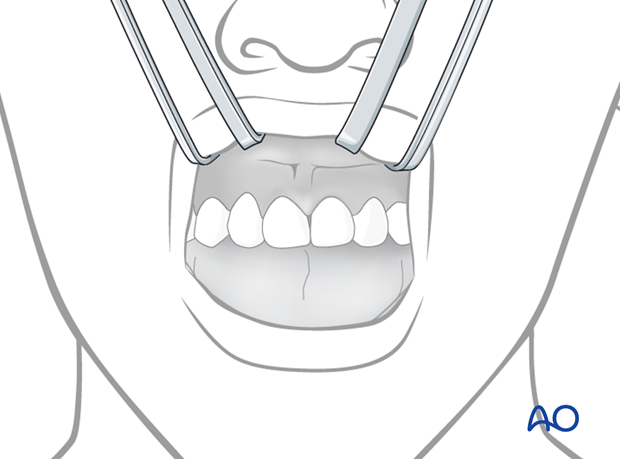
Splint removal
After the fixation period (4 weeks) the resin can be peeled off with a dental scaler or removed with a burr. The tooth must be supported by digital axial pressure during this procedure.
3. Orthodontic repositioning
Principles
By means of orthodontic appliance anchored to neighboring two or preferably more teeth on each side of the traumatized tooth, the intruded tooth may be gently pulled towards its proper position by means of elastic traction. The whole procedure requires at least 3–4 weeks. The force of extrusion should be kept low, and the procedure requires a close follow-up scheme.
Application of bracket
The crown of the intruded tooth is exposed. After etching, rinsing, and drying of the enamel surface of the intruded tooth, a bracket is bonded to the enamel surface.
Anchorage
After etching, rinsing, and drying of the enamel surfaces of at least two neighboring teeth on each side of the intruded tooth, a metal thread is bonded for anchorage
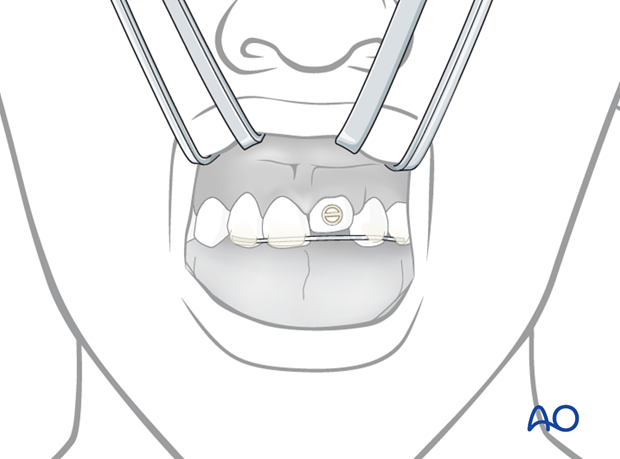
Elastic traction
Elastic traction is established between the anchoring rod and the bracket on the tooth. Elastics should be checked and replaced once a week until successful repositioning has been achieved.
The repositioning needs at least 3–4 weeks. The force of extrusion should be kept moderate, and the procedure requires a close follow-up.
Removal of fixation devices
The resin can be peeled off with a dental scaler or removed with a burr. The tooth must be supported by axial digital pressure during this procedure.
Completed repositioning
Illustration shows completed repositioning.
4. Await spontaneous eruption
Indications for this procedure are primary and adolescent teeth with incomplete root formation and moderate intrusion.
Spontaneous re-eruption should start to occur within 3–4 weeks. If this does not occur within a reasonable time frame, orthodontic repositioning may be the treatment of choice.
5. Aftercare following treatment of intrusion
Optimal oral hygiene is essential including tooth brushing using a soft tooth-brush and mouth rinsing with 0.1 % chlorhexidine twice a day. This is especially important until completion of gingival healing.
In case of undesired signs and symptoms related to the fixation appliance, the patient is encouraged to seek help as soon as possible.
Aftercare includes endodontic treatment in all teeth with completed root formation and in those teeth with incomplete root formation which develop pulp necrosis.
Follow-up
This type of injury is prone to show late complications (ankylosis) and need at least 5 years of follow-up.
Diet
Patients are encouraged to restrict themselves to a semi-solid diet and avoid clenching and any other traumatic overload to the traumatized tooth for a period of up to 4 weeks posttrauma.
Further treatment
Further dental treatment may be needed as elective procedures, for example management of crown fractures, discoloration, porcelain restorations, etc .













