Complications
1. General considerations
Complications can be of many types: pulp necrosis, root resorption, and loss of supporting bone. Any of those complications can lead to the ultimate loss of the affected tooth. Complications such as compromised root development, and malformation of dental hard tissue are less prone to premature loss of the traumatized tooth.
2. Pulp healing complications
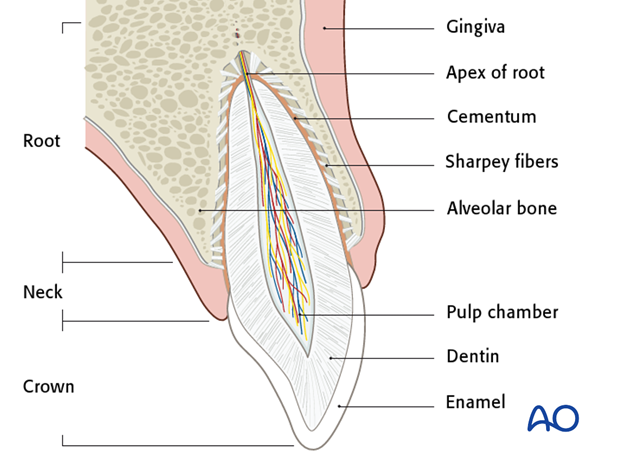
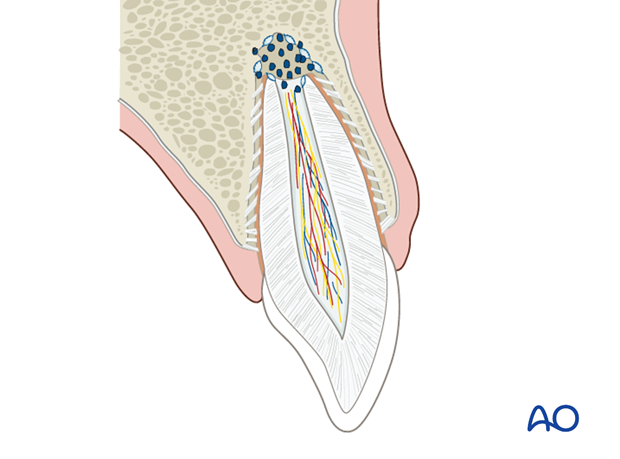
The pulp frequently suffers ischemic injury after luxation injuries due to disruption of the neurovascular supply at the apical foramen. Successful healing takes place by revascularization and reinnervation from the apical socket. Due to the dead-end structure of a pulp canal, this process is very sensitive and the chance of successful outcome is related to the size of the apical foramen. That is, teeth with incomplete root formation have an optimal chance of healing, whereas teeth with complete root formation most often suffer a pulp necrosis. In the ischemic state, the pulp is extremely vulnerable to bacterial contamination that may arise from three sources:
- Leaks in the periodontal ligament due to luxation injuries
- Invasion through dentinal tubules
- Blood borne bacteria
Bacterial invasion via the periodontal ligament can be reduced by timely repositioning and gentle but adequate cleansing of exposed root surfaces before repositioning.
Note: Do not harm chemically or mechanically the periodontal ligament and do not let it dry out. (LINK to treatment of avulsed teeth)
Furthermore, splinting devices should keep clear of the gingival margin. Luxated teeth should not be used for anchorage of dental arch bars. After initial treatment, optimal oral hygiene is essential including tooth brushing using a soft tooth brush and mouth rinse with 0.1 % chlorhexidine twice a day. This is especially important in the first week until completion of gingival healing.
Exposed dentin tubules should be sealed whenever feasible, eg, using glass ionomer cement.
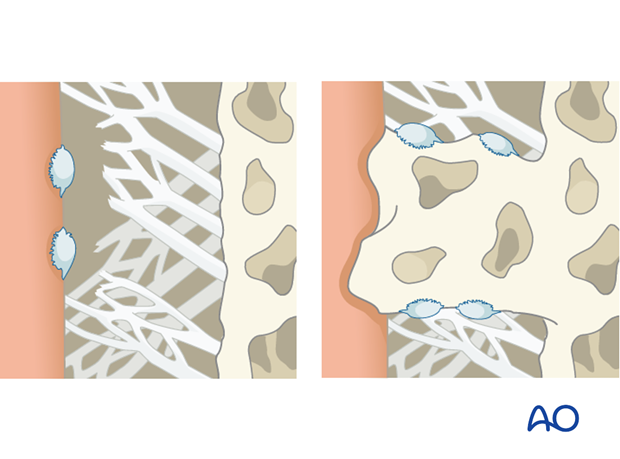
3. Periodontal healing complications: Repair-related resorption (surface resorption)
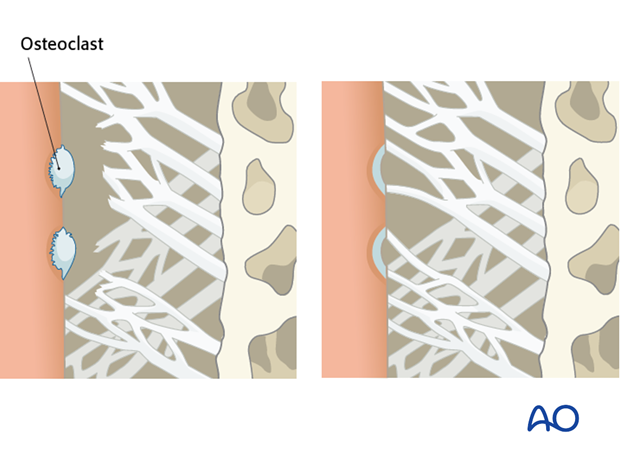
Repair-related resorption (surface resorption) is a frequent resorption type which presents itself as small cavities on the root surface that heal by new formation of cementum accommodating the reformed periodontal ligament fibers. These areas represent minor ischemic injuries to the periodontal ligament which cause resorption of soft tissue by macrophages and hard tissues by osteoclasts. When that has occurred, exposed cementum and dentin release growth factors which trigger periodontal ligament specific cells to repair the site. This type of resorption can sometimes be seen on x-ray if concentrated on the apex but has no practical importance since resorption cavities are self-healing and do not represent a threat to the survival of the tooth.
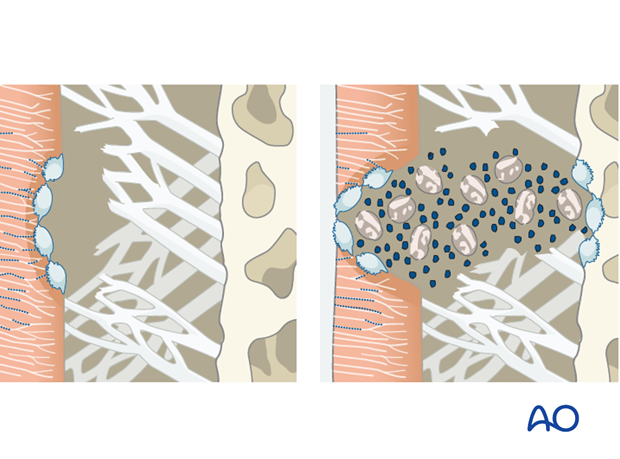
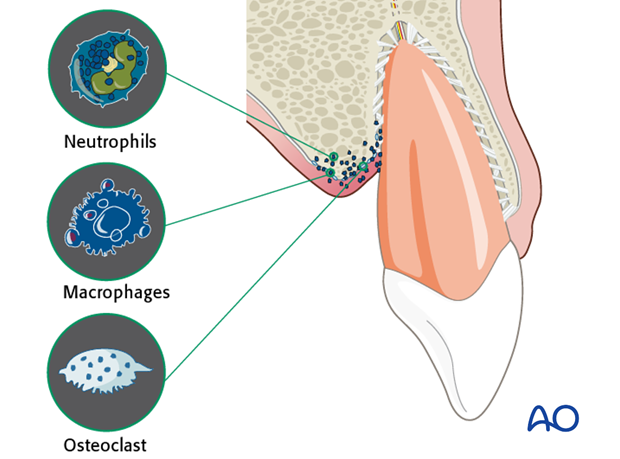
4. Periodontal healing complications: Infection-related resorption (inflammatory resorption)
Infection-related resorption (inflammatory resorption) is a more severe type of resorption. This type of resorption starts out similar to repair-related resorption. A leakage of toxins from the infected pulp through dentinal tubules will start a chain reaction stimulating osteoclasts to resorb not only from the cementum and dentin but also alveolar bone. In this way an aggressive resorption process is started which in a few months can lead to loss of most of the root structure.
On x-ray, it is seen as excavations on the root surface in connection with excavations on the adjacent alveolar bone taken up by resorptive granulation tissue. The resorption will be visible on x-ray after 2 to 3 weeks. It is important to consider that proper endodontic intervention can either prevent this complication or control if it has occurred. Proper follow-up is mandatory in all cases diagnosed as infection-related resorption (intrusions and avulsions with subsequent replantation).
5. Periodontal healing complications: Replacement osseous resorption (ankylosis)
Replacement osseous resorption (ankylosis) is the result of extensive damage to the periodontal ligament whereby the cells keeping osteoclasts and osteoblasts at a distance are killed (loss of homeostasis in the periodontal ligament). In this situation, the injured tissue in the socket leads to socket healing whereby a bony bridge is formed between the socket wall and the root surface. The root is now integrated in bone and it will resorb along with bone remodeling. This process might lead to infraposition where the tooth is not in alignment in the dental arch (below the occlusal plane) and migration of adjacent teeth into the injury site. The resorption rate is especially high in adolescence.
The types of injuries that exhibit this complication frequently are intrusion and avulsion with subsequent replantation. To prevent replacement osseous resorption, it is important not to use fixation devices which create compression in an already damaged periodontal ligament. Therefore, particularly luxated teeth, replanted teeth, and other teeth with periodontal ligament damage should not be included in the fixation of dental arch bars.
There is no effective treatment of this resorption type. However, the tooth can be used to temporarily maintain the space in growing individuals and as a method of preservation of alveolar bone (“no teeth, no bone”). Removal of the crown just below the alveolar crest (coronectomy) should be carried out when ankylosed roots are left in place in growing individuals to enable bony and soft-tissue healing to cover the root as a result of the normal alveolar process appositional growth.
6. Alveolar bone healing complications
Some injury types lead to severe crushing of bone in the cervical region of the tooth. In such situations, the healing of associated gingival lesions may result in sulcular epithelial downgrowth reducing periodontal support of the tooth.
Sequestration (exfoliation of necrotic bone) of marginal bone fragments due to trauma is infrequent but occasionally occurs after tooth intrusions and alveolar fractures. More often, sequestration or bone loss occurs after inappropriate exposure of bony fragments. This emphasizes the importance of informed dentoalveolar trauma management.
7. Compromised root development
Compromised root development may happen when a luxation injury results in incomplete, arrested and/or distorted root formation. In this situation, injury to the tooth root-forming structures (Hertwig’s epithelial root sheath) may compromise further root formation.
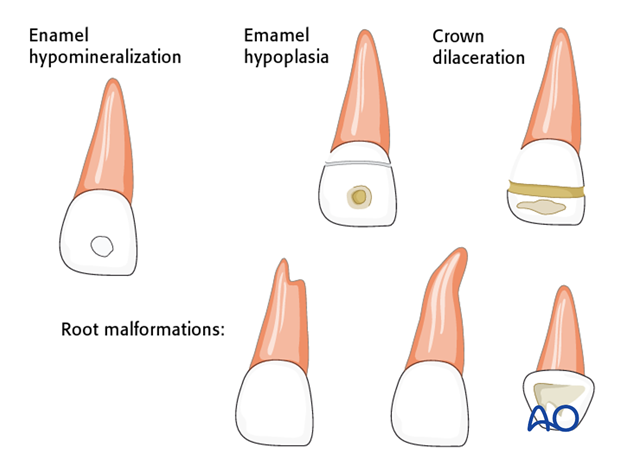
8. Disturbance in tooth development
This may occur if a jaw or alveolar fracture involves a developing tooth, and after intrusion or avulsion injuries of primary teeth. Such injury may range from disturbance of enamel formation or maturation. More serious sequelae may result in malformation of the major structure of the entire crown and/or root.