One stage nasolabial flap
1. Introduction
One stage nasolabial flaps are used for small superficial defects within the sidewall or nasal ala.
In this authors experience, the use of local nasal flaps (bilobed or dorsonasal flaps) may lead to adjacent landmark distortion. Because there is limited excess lax skin within the nasal surface, there is not enough skin to share. Skin must be added to the nasal surface, not redistributed. This risk can be minimized by using the one stage nasolabial flap which adds cheek skin to the nose.

Principles of reconstruction
Each defect is different but each reconstruction is simplified because the "Normal" never changes so the principles of repair remain the same. The contralateral normal remains as a visible comparison. If the contralateral normal is unavailable, the ideal is used as a guide.
The face can be described in regional units characterized by:
• Skin quality
• Border outline
• 3 dimensional contour
Anaesthesia
This procedure is commonly performed under general anaesthesia to minimize soft tissue distortion and vasoconstriction associated with local anaesthesia injection.
Smaller defect can be repaired under local anesthesia with or without sedation or general anesthesia.
The fluid volume of local anaesthetic alters the dimension, thickness, and position of both the donor tissues and recipient site. The blanching caused by epinephrine will make evaluation of tissue vascularity difficult intraoperatively.
2. Resection
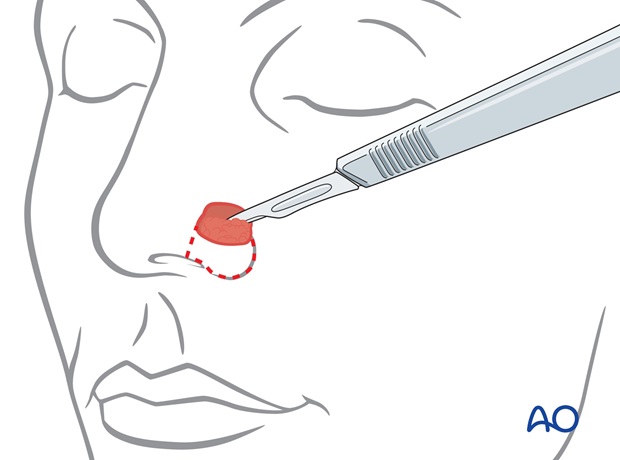
If an initial excision is required to treat skin cancer, the tumor is excised utilizing standard excisional margins, verified by frozen section by the operating surgeon or by the Mohs technique.

3. Reconstruction
Flap design
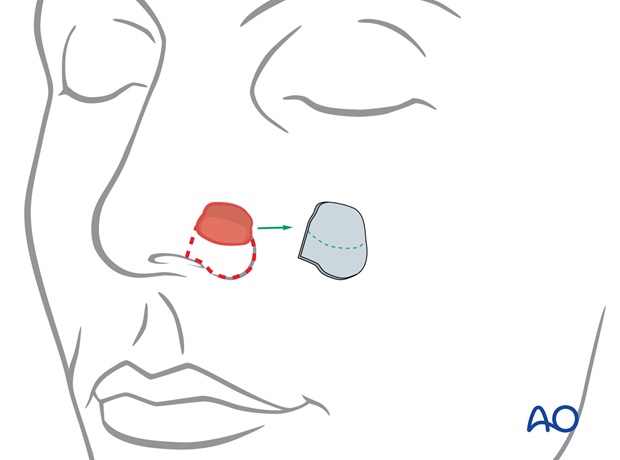
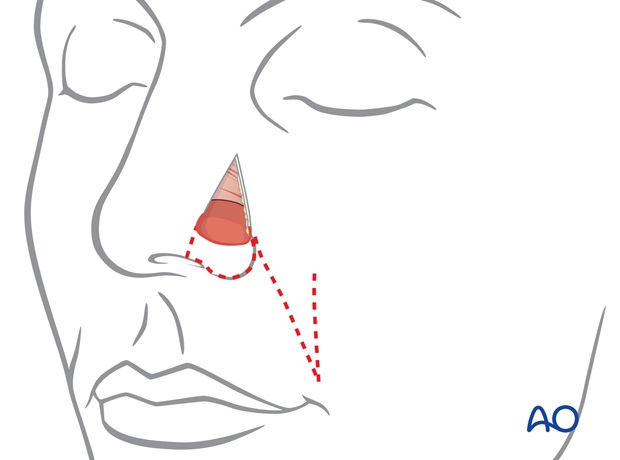
A template or pattern of the area of the defect, with or without additional skin to the rim margin, is marked for excision.
A clean surgical wound is prepared by excision of the wound edges and debridement of any injured tissues or granulation tissues.
The template is positioned immediately adjacent to the nasolabial fold, ensuring an appropriate arc of rotation from the donor to the recipient site.
A distal "dog ear" excision is outlined.
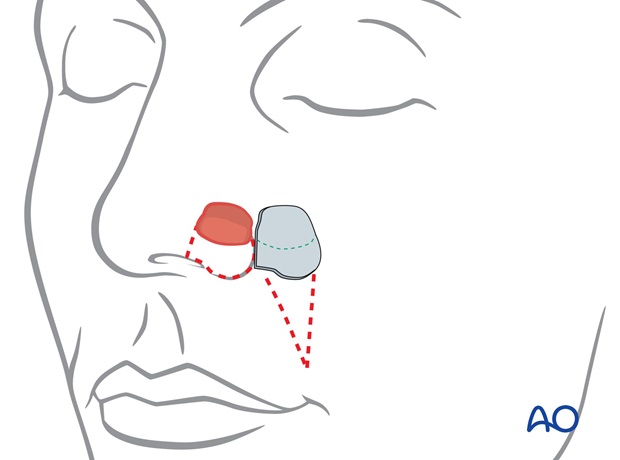
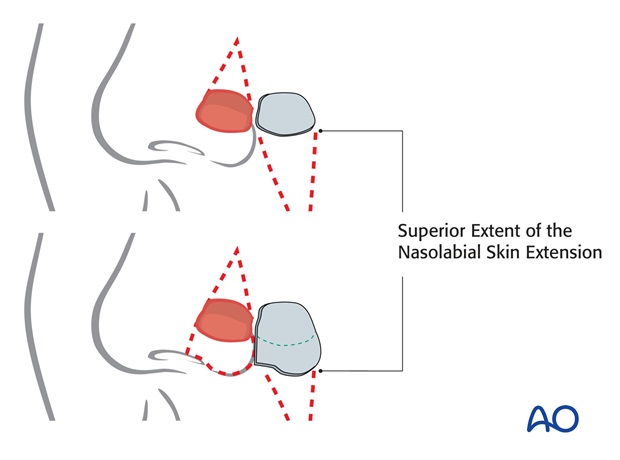
A burrows triangle is marked superior to the defect for excision to permit advancement of the cheek flap onto the nasal wall.
Pitfall: The nasolabial skin is transferred as an extension of an advancing cheek flap and the lateral incision should be limited superiorly to avoid devascularization of the flap.
Preparation of recipient site
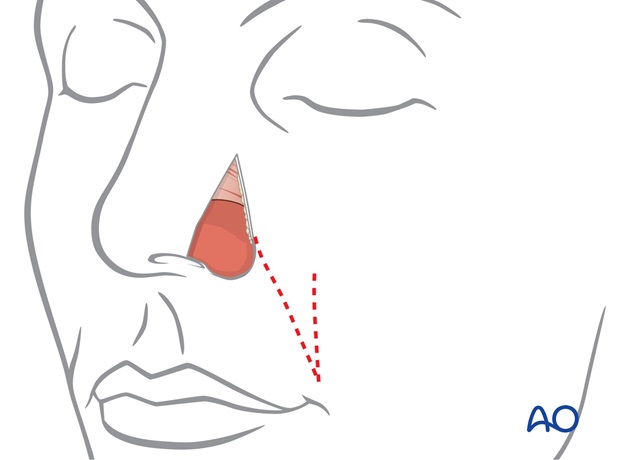
Skin and subcutaneous fat is excised within the burrows triangle.
If desired, skin remaining between the nostril margin and the defect can be excised to position the inferior border scar along the nostril margin.
Preparation of alar support
Normally the ala contains no cartilage, but an alar margin Batten graft must be placed into a large deep defect of the ala to support, shape and brace the reconstructed ala postoperatively, even for more limited superficial defects.
Although septal or rib cartilage can be utilized, conchal cartilage is ideal because of its natural curvature.
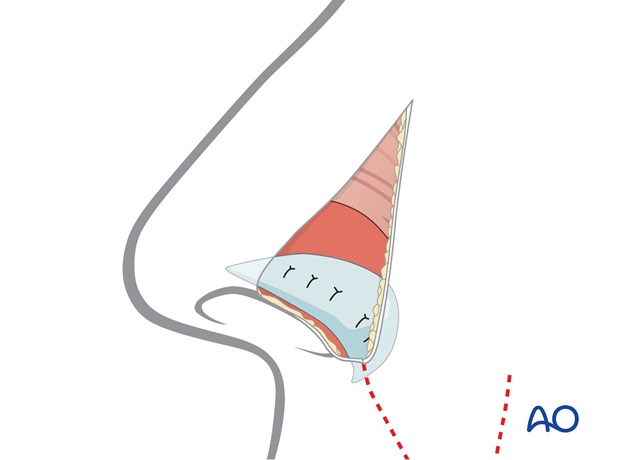
The conchal cartilage is harvested through a postauricular incision.
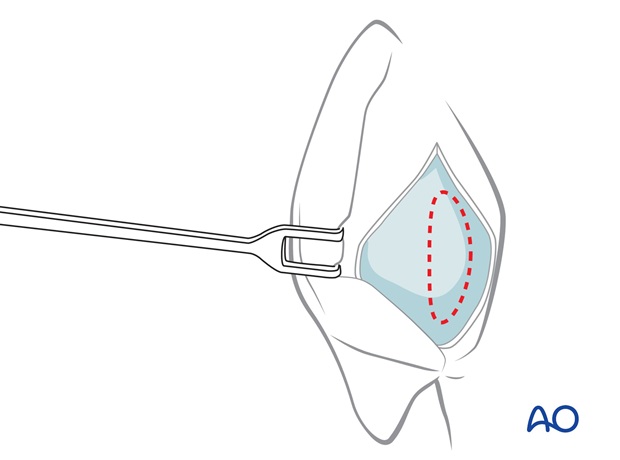
The template of the contralateral ala is used as a guide to create a nostril margin graft of the correct dimension and border outline.
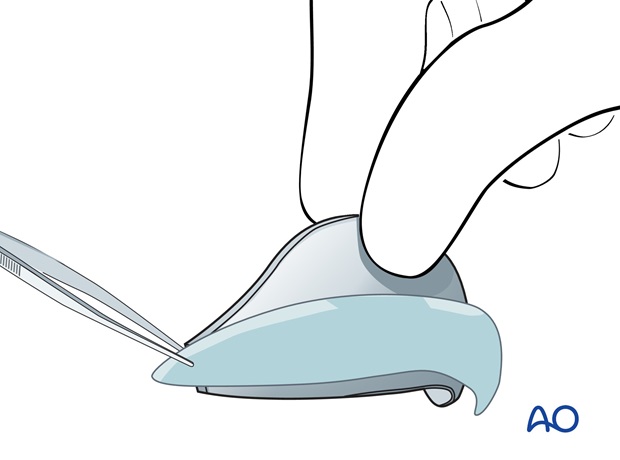
The dimension of the graft is extended a few mm medially and laterally to allow its fixation in small subcutaneous pockets created laterally within the soft tissues of the alar base and medially under the skin of the tip.
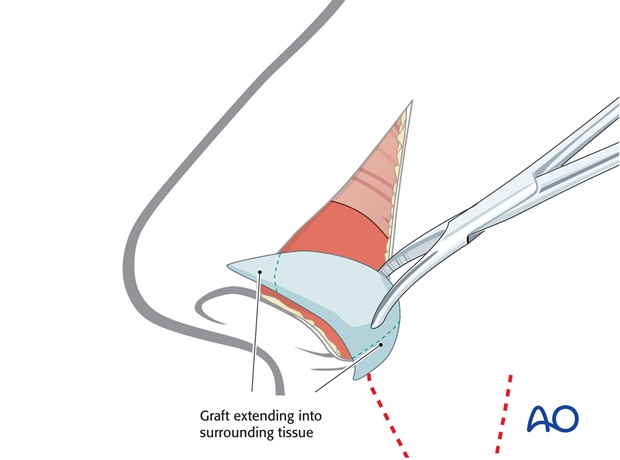
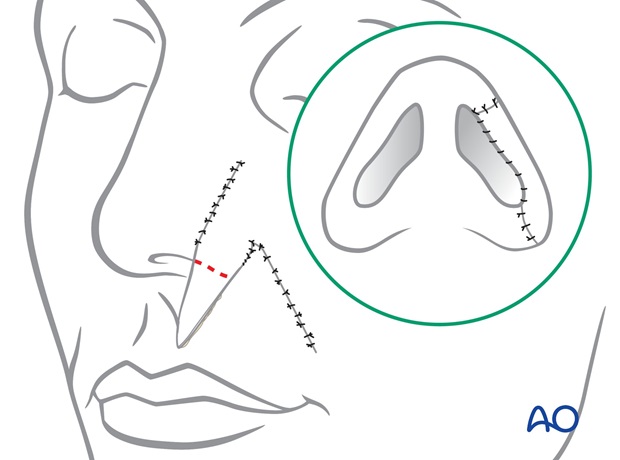
The ear cartilage graft is fixed into the pockets with percutaneous quilting sutures medially and laterally. The graft itself is sutured to the underlying raw lining surface.
Flap inset
Medial cheek skin is elevated with a few mm of subcutaneous fat and advanced onto the nose, carrying the distal extension to cover the defect
The superior extent of the nasolabial skin extension is incised laterally only enough to permit its rotation and advancement to the recipient site.
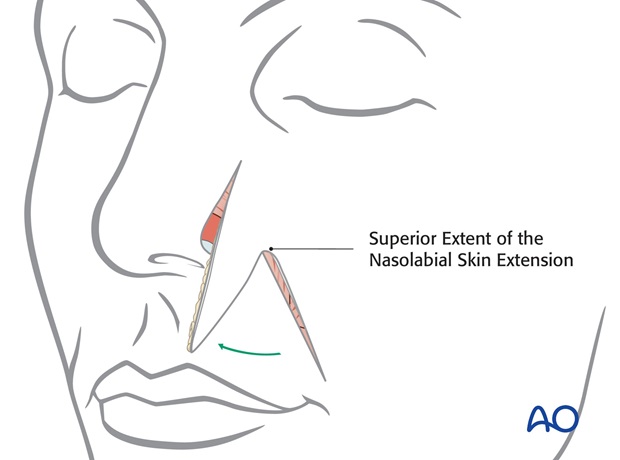
The cheek flap is advanced and fixed on its deep surface to the naso facial groove, to minimize lateral tension.

The advanced cheek flap is fixed with deep sutures in the naso-facial sulcus to minimize tension of the nose and the flap extension.
The wound edges are then closed in layers with subcuticular sutures and skin sutures.
If well vascularized, the deep surface of the flap can be fixed to the soft tissues of the alar crease to restore its contour.
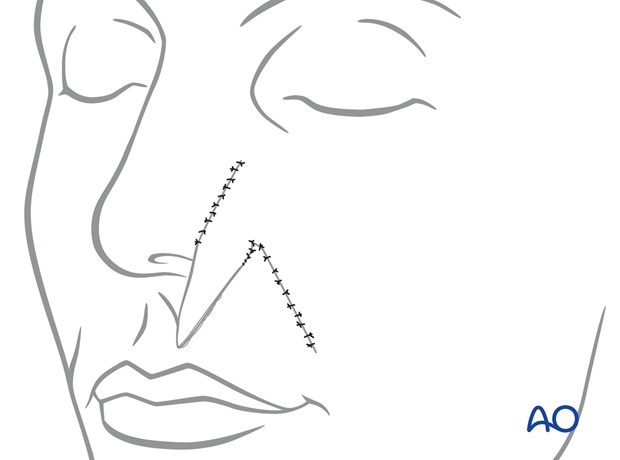
The excess skin of the "dog ear" is trimmed along the nostril margin and the flap inset along the nostril margin.
Revision surgery
Almost all major nasal reconstruction will require a revision procedure four months after the initial reconstruction to improve the final result.

Case
Pre-and postoperative photographs of a small superficial defect repaired using a one stage nasolabial flap.

4. Aftercare following nose reconstruction
Skin graft
The bolus skin graft dressing should be kept dry. The forehead donor site can be washed within 24 h.
Forehead nasal reconstructions
Routine showering is permitted within 24 hours of all surgical sites. Dressings are worn at the discretion of the patient.
Quilting sutures are removed after 48h. Routine skin sutures are removed after 7 days. Sun exposure is avoided for several months after surgery.













