Two stage forehead flap - Ala reconstruction
1. Introduction
Single subunit defects of the ala that require only modest skin resurfacing and limited cartilage replacement can be resurfaced with forehead skin transferred in two stages.
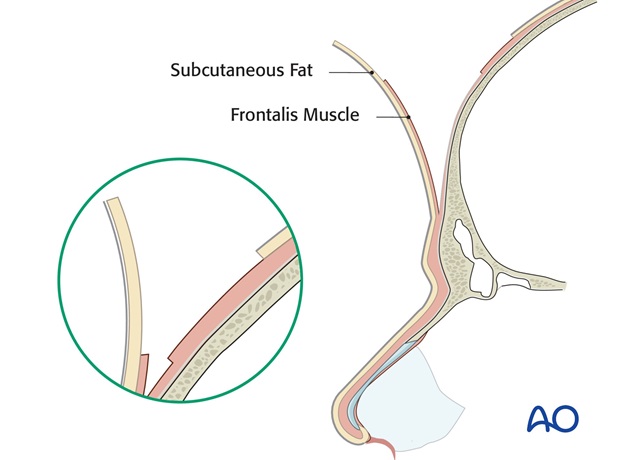
At the time of flap transfer, excessive subcutaneous fat and frontalis muscle of the forehead flap are excised from the distal flap to create a skin flap of a thickness similar to that of the missing skin of the nose.
Principles of reconstruction
Each defect is different but each reconstruction is simplified because the "Normal" never changes so the principles of repair remain the same. The contralateral normal remains as a visible comparison. If the contralateral normal is unavailable, the ideal is used as a guide.
The face can be described in regional units characterized by:
- Skin quality
- Border outline
- 3 dimensional contour
The principles of nasal reconstruction which apply to large deep defect which will be resurfaced with a flap are:
- Recreate nasal subunits, not just fill the defect.
- Alter the wound in site, size and depth to improve the final result
- If appropriate, excise residual normal skin within the subunit to replace missing skin as a unit, rather than as a patch (subunit principle)
- Use the contralateral Normal or the Ideal as a guide
- Replace missing tissues exactly
- Employ surgical templates
- Build on a stable platform
Subunit principle: If a defect encompasses more than 50 % of a convex subunit – tip or ala - remaining normal skin is excised within the subunit and the entire subunit is resurfaced with a subunit flap. This positions final border scars in the junctions between adjacent subunits and harnesses flap trapdoor contraction and postoperative pin cushioning, and in combination with shaped underlying cartilage support, augments the shape of underlying cartilage support over the entire subunit.
Anaesthesia
This procedure is performed under general anaesthesia to minimize soft tissue distortion and vasoconstriction associated with local anaesthetic injection.
The fluid volume of local anaesthetic alters the dimension, thickness, and position of both the donor tissues and recipient site. The blanching caused by epinephrine will make intraoperative evaluation of tissue vascularity difficult.
2. Resection
If an initial excision is required to treat skin cancer, the tumor is excised utilizing standard excisional margins, verified by frozen section by the operating surgeon or the operating Mohs surgeon.
3. Stage 1: Reconstruction of a deep alar defect
Template preparation
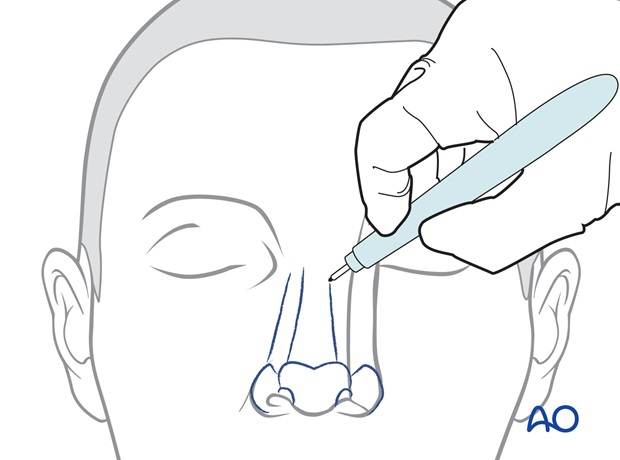
The subunits of the nose and regional units of the face are marked with ink.
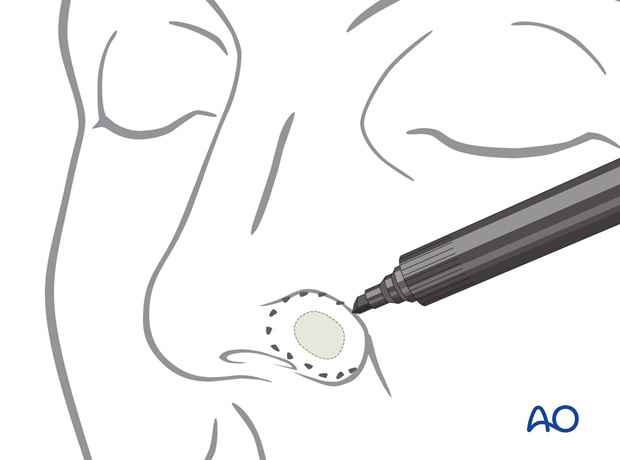
A template of the intact contralateral alar subunit is created using quarter inch adhesive paper tape and collodion.
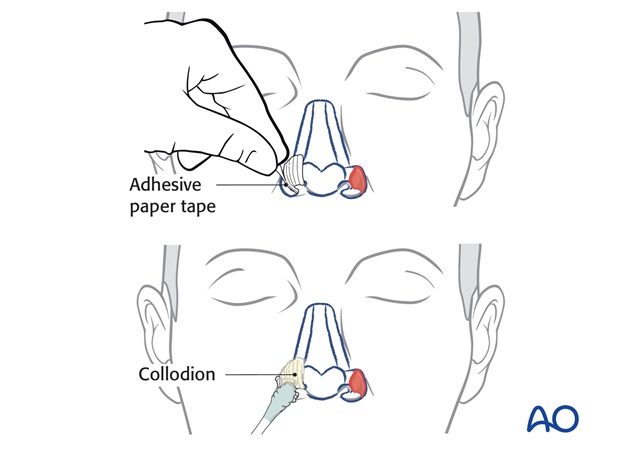
The excess paper tape is trimmed to create an exact pattern in dimension and border outline of the skin required to resurface the entire alar subunit.
The outline of the paper template is transferred to the foil of a suture pack to create a more mechanically stable pattern.
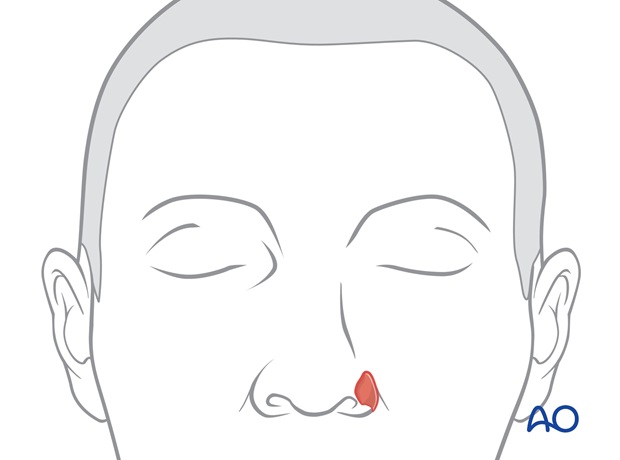
Excision of residual skin
If a subunit excision is planned, residual normal skin within the subunit is excised.
Preparation of alar support
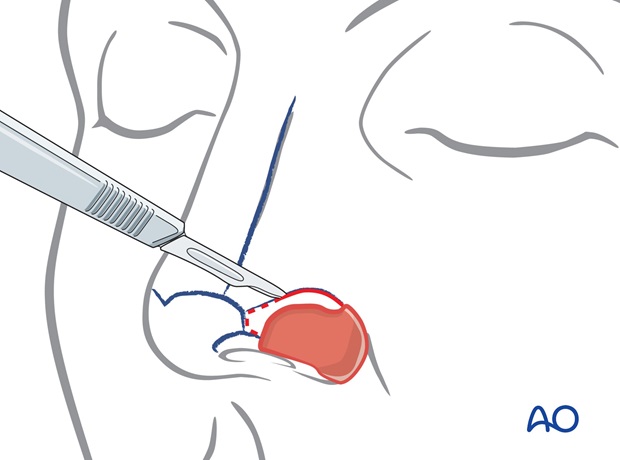
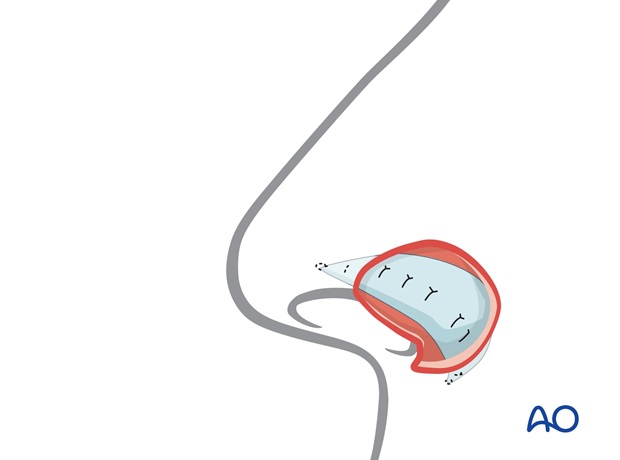
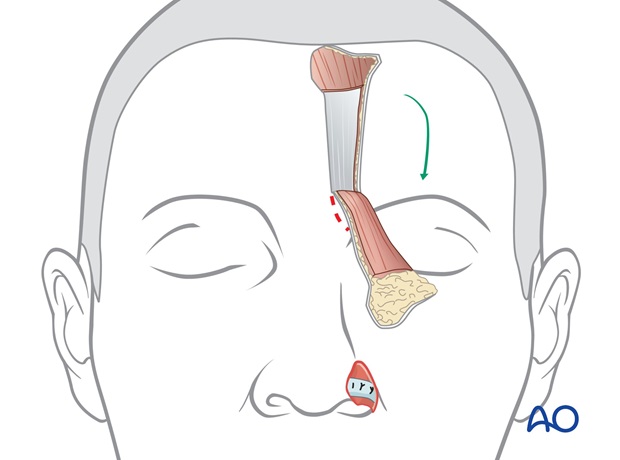
Normally the ala contains no cartilage, but an alar margin Batten graft must be placed into a large deep defect of the ala to support, shape and brace the reconstructed ala postoperatively.
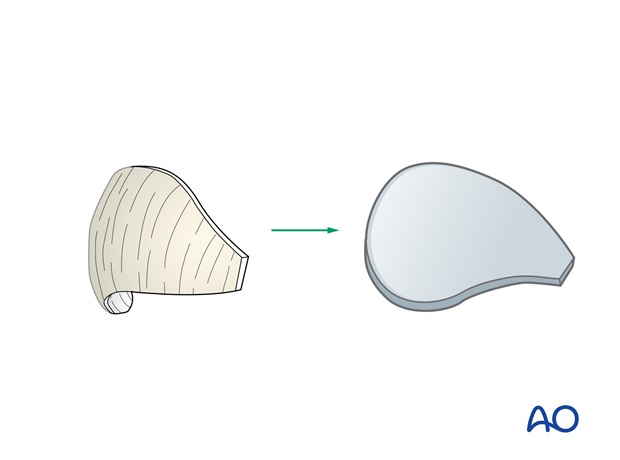
Although septal or rib cartilage can be utilized, conchal cartilage is ideal because of its natural curvature.
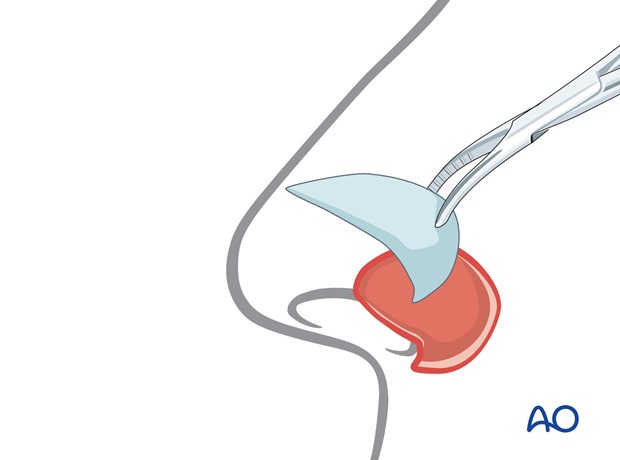
Conchal cartilage is harvested through a postauricular incision.
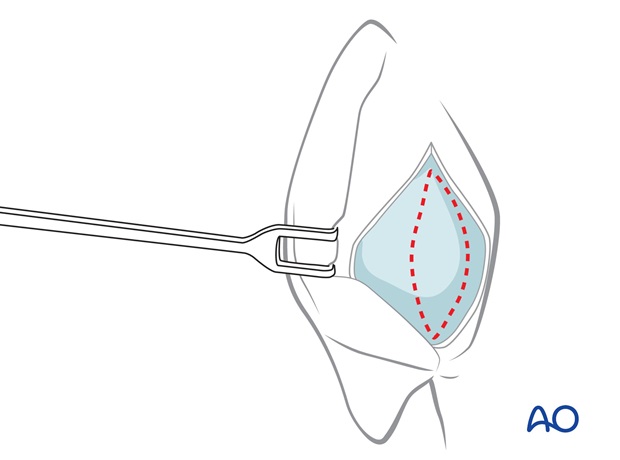
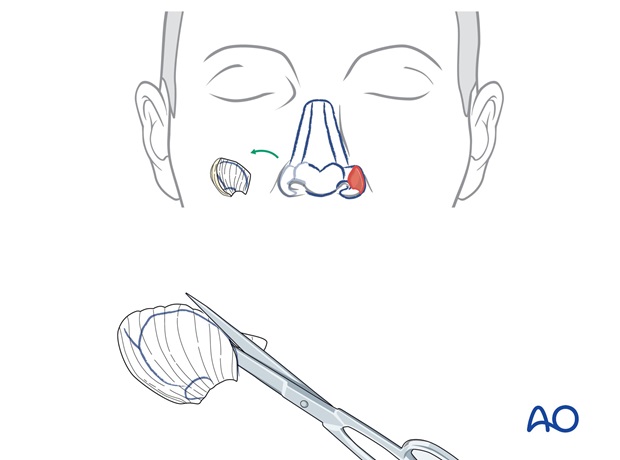
The template of the contralateral ala is used as a guide to design a nostril margin graft with the correct dimension and border outline.
The dimension of the graft is extended a few mm medially and laterally to allow its fixation in small subcutaneous pockets created laterally within the soft tissues of the alar base and medially under the skin of the tip.
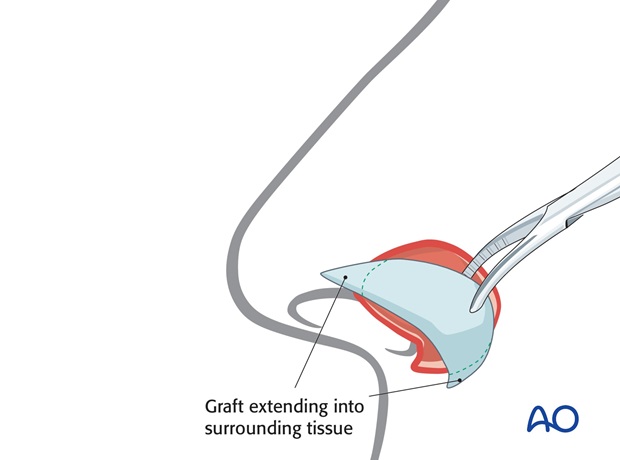
The ear cartilage graft is fixed into the pockets with percutaneous quilting sutures medially and laterally. The graft itself is sutured to the underlying raw lining surface.
Design of paramedian forehead flap
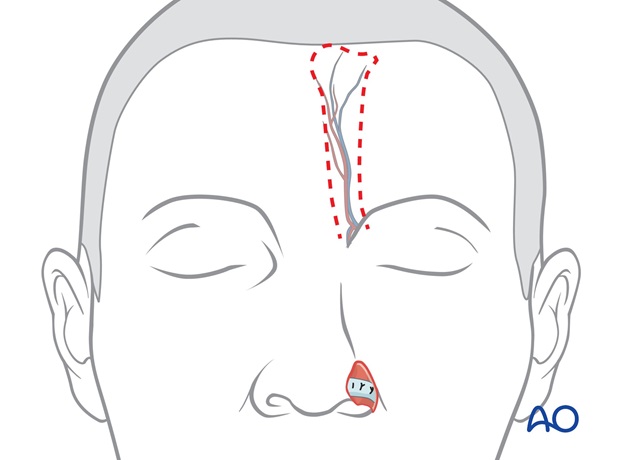
The exact dimension and outline of the missing nasal skin which will be replaced with the forehead flap is designed using the alar template.
The contralateral alar template is a mirror image of the missing ala and must be flipped over (180°) to correctly orient the flap to the recipient site.
The template is positioned under the hairline directly superiorly to its supratrochlear pedicle, which is located a few mm lateral to the frown crease (verified by doppler).
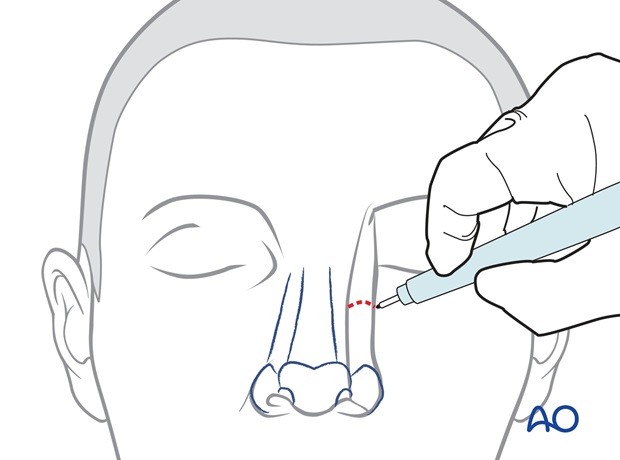
The paramedian flap is perfused by the supratrochlear vessels and can be based on either side of the forehead. Unilateral defects are more easily resurfaced with the ipsilateral flap because its pedicle is closer to the defect.
Either the right or left pedicle can be chosen for midline defects.
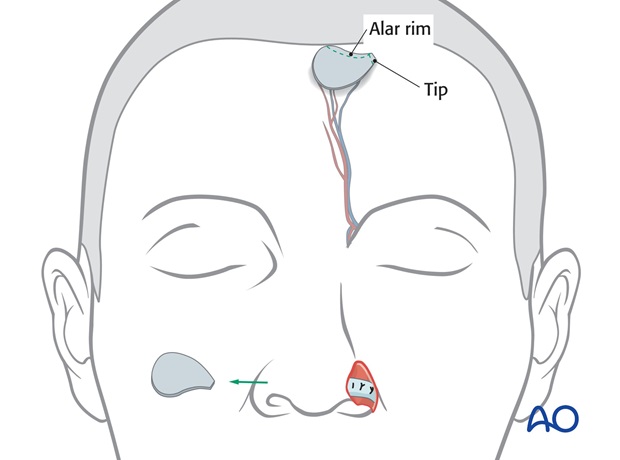
Centered over the supratrochlear vessels, the flap’s pedicle is drawn inferiorly through the medial eyebrow, narrowing to 1.2 to 1.5 cm in width at the pedicle base.
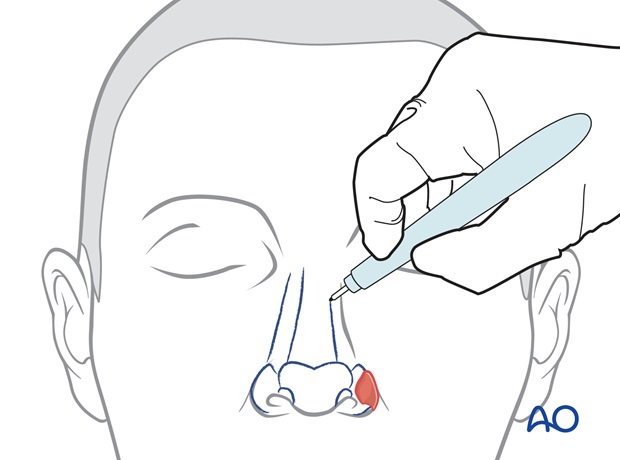
Flap harvest
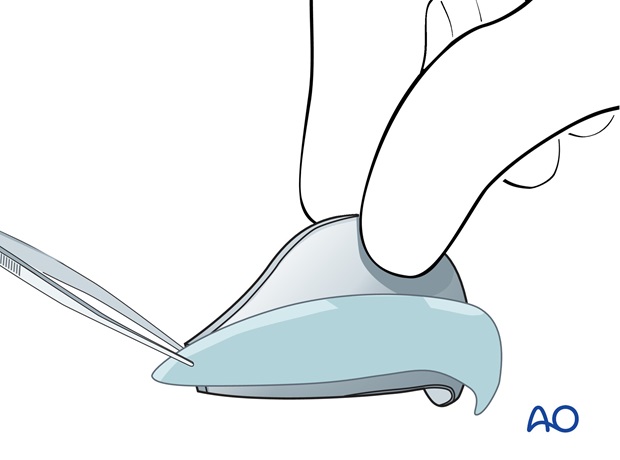
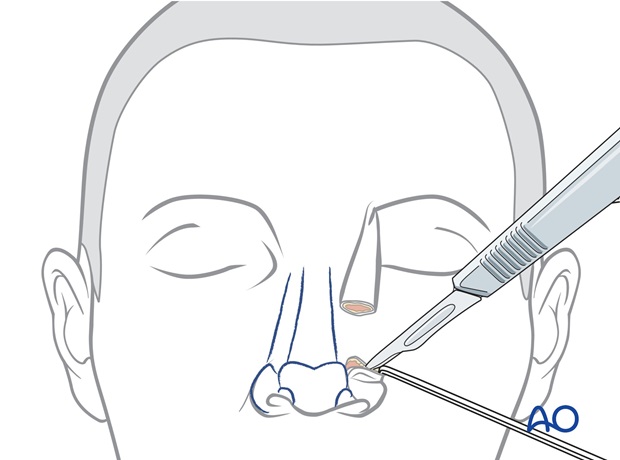
The border of the flap is incised. To thin the distal flap, the distal 1.5 cm of skin is elevated with 2-3 mm of subcutaneous fat, leaving underlying additional subcutaneous fat and frontalis muscle intact over the periosteum.
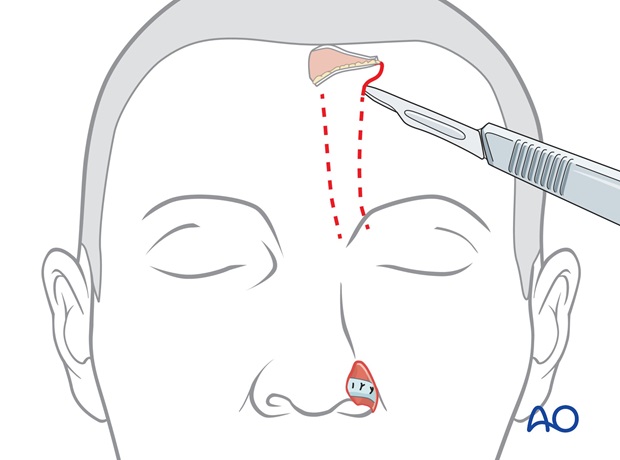
The dissection then passes through the frontalis muscle and the flap is elevated from distal to proximal over the periosteum to its pedicle base.
The flaps base is incised through the medial eyebrow spreading the corrugator muscle until the flap can be rotated medially to cover the nasal defect without tension.
Closure of donor site defect
The scalp dog ear is excised and the forehead is widely undermined.
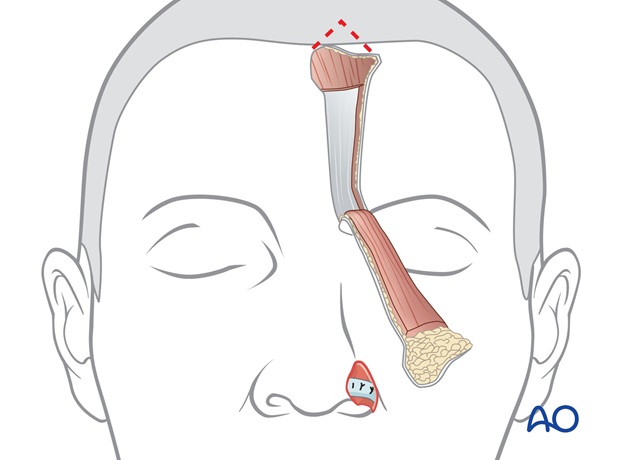
The forehead defect is closed in layers.
Flap inset
The forehead flap is sutured into the recipient site with a single layer of sutures.
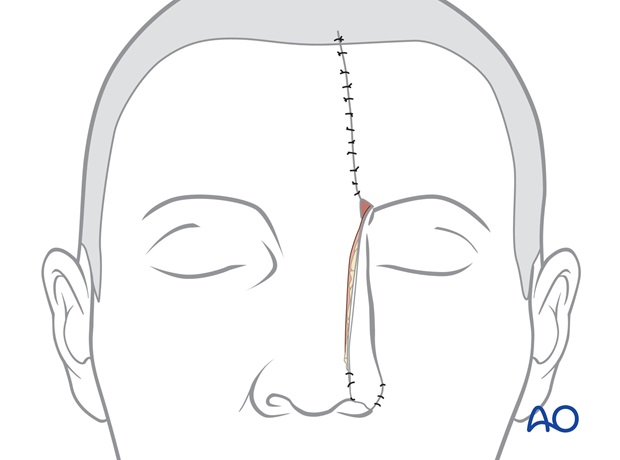
A full thickness skin graft harvested from the groin is placed on the raw deep surface of the pedicle for cleanliness.
The pedicle is divided one month later.
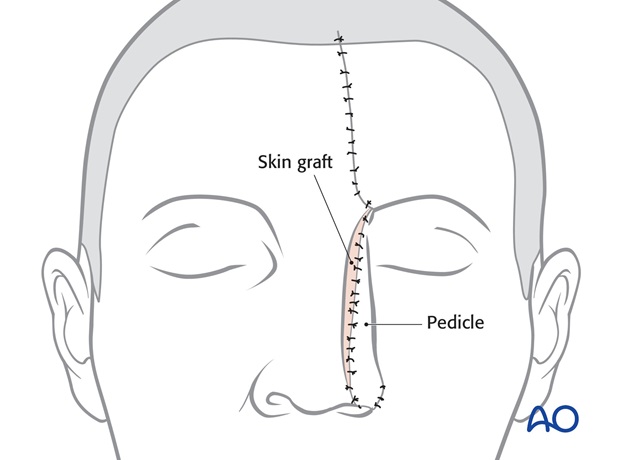
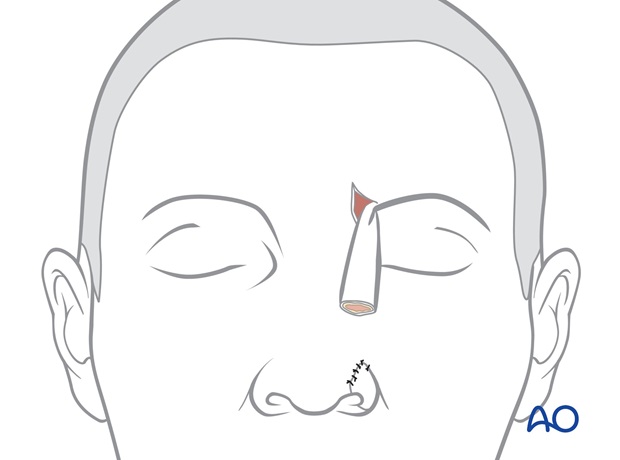
4. Stage 2: Pedicle division
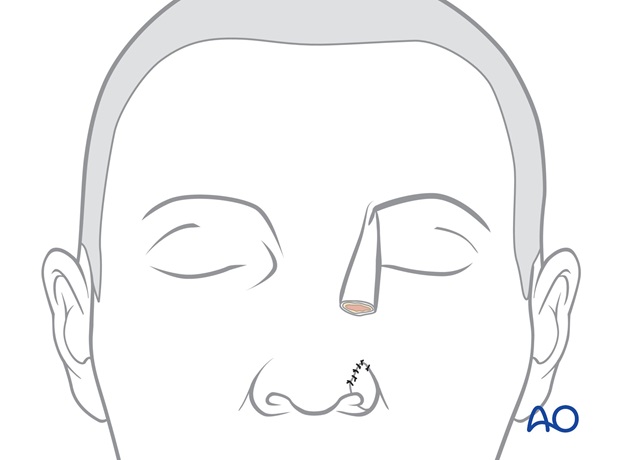
The regional units of the nose are marked with ink.
The site of pedicle division is marked, leaving excess tissue that can be trimmed at the time of fine tuning the reconstructed subunit.
The pedicle is divided. The skin of the nasal inset is elevated with 2-3 mm of subcutaneous over the superior aspect of the reconstructed ala. Underlying subcutaneous fat or excess cartilage is excised to sculpt a convex alar contour.
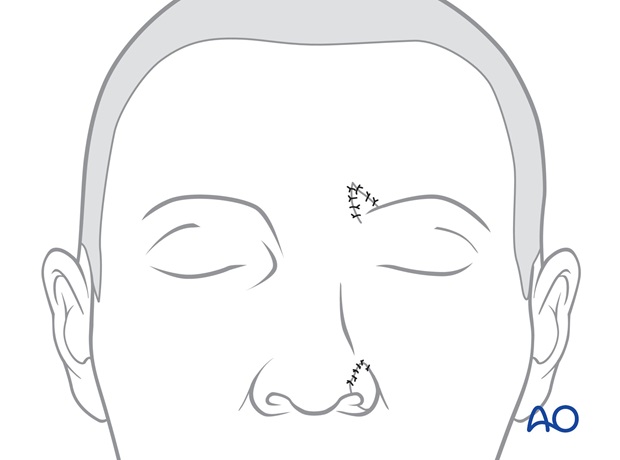
Excess forehead skin is trimmed and the forehead skin inset completed with skin sutures.
Forehead closure
The inferior part of the forehead scar through the medial eyebrow is reopened.
The skin of the proximal forehead pedicle is elevated with several mm of subcutaneous fat from the underlying excess soft tissue and previous skin graft on the deep surface of the proximal pedicle.
The excess underlying soft tissue bulk is excised to sculpt an inset for the medial brow inset.
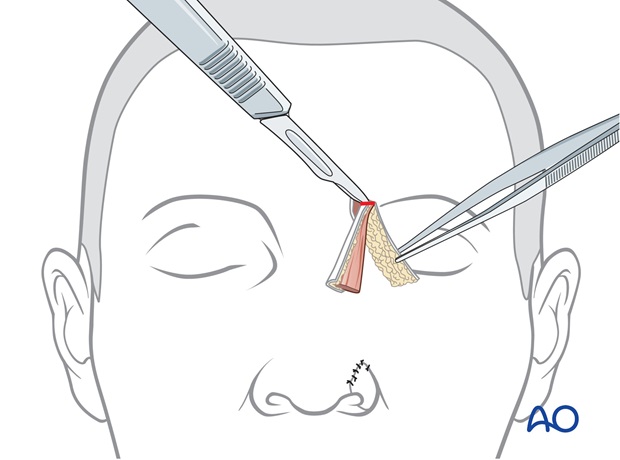
The skin of the proximal pedicle is trimmed, returning the medial eyebrow to its normal position and inset as a small inverted V whose scars simulate the normal frown crease.

It is fixed in place with a temporary quilting suture and a layered skin closure.
Revision surgery
Almost all major nasal reconstruction will require a revision procedure four months after the initial reconstruction to improve the final result.

5. Aftercare following nose reconstruction
Skin graft
The bolus skin graft dressing should be kept dry. The forehead donor site can be washed within 24 h.
Forehead nasal reconstructions
Routine showering is permitted within 24 hours of all surgical sites. Dressings are worn at the discretion of the patient.
Quilting sutures are removed after 48h. Routine skin sutures are removed after 7 days. Sun exposure is avoided for several months after surgery.













