Patient evaluation and management
1. Management of the paralyzed face
The objectives in the management of the paralyzed face are to provide:
- Symmetry at rest
- Facial tone
- Voluntary movement
- Symmetry with movement
- Spontaneous movement
- Reduction of synkinesis
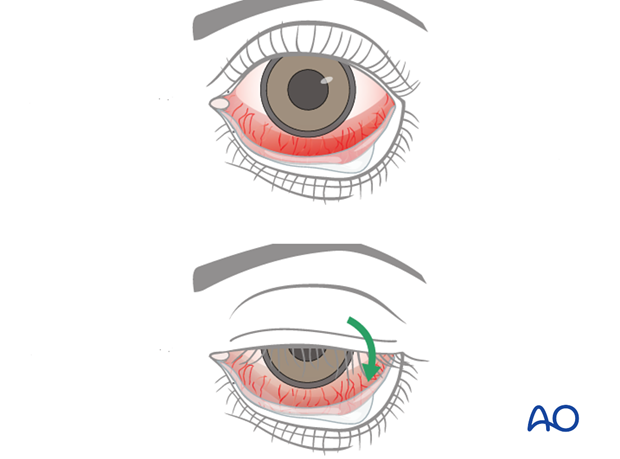
The immediate priority in managing a patient with facial paralysis is ensuring adequate corneal protection.
It is important to maintain lubrication and protection of the eye. Lubrication consists of natural tear substitutes during the day and ointment based lubricants during sleep, often together with taping the eyelid closed.
Physical protection through eyewear may be necessary depending on occupation and environmental conditions.
Lateral tarsorrhaphy should be considered in most situations as a temporary and/or preemptive measure prior to definitive procedure to improve eyelid function and ensure corneal protection. A detailed description of lateral tarsorrhaphy can be found in the dedicated treatment section under "reversible paralysis".
Once the eye is deemed protected, the following clinical variables need to be determined in order to develop a treatment strategy:
- Reversible vs irreversible paralysis
- Upper face (eye) paralysis
- Lower face (mouth) paralysis
- Existing available anatomy that can be used for reconstruction (e.g. tendons, masseter muscle, temporalis muscle, trigeminal nerve)
- Patient variables (age, general health, radiation therapy)
- Prognosis
Treatment for each patient must be individualized, and is dependent on:
- Patient history (including the cause of facial paralysis)
- Physical examination
- Investigation
- Patient expectations and motivation
2. Patient history
The following parameters should be analyzed:
- Cause of paralysis
- Duration of paralysis
- Changes over time
- Prior surgeries and treatments (radiation/scar)
- Patient age and overall health
- Specific patient complaints/concerns
Cause of paralysis
In most situations, the cause of paralysis is well defined. The most common cause of facial paralysis is Bell's palsy. Nevertheless, Bell's palsy is a very specific clinical diagnosis and is not synonymous with all cases of facial paralysis.
Duration of paralysis
Different reconstructive options can be selected depending on the duration of paralysis.
Intraoperative direct nerve stimulation may be possible up to 7 days from the time of a transection injury. This may make early exploration and repair advantageous.
The critical window of opportunity to reinnervate the muscles of facial movement in long standing paralysis is 18-24 months.
Changes over time
It is necessary to monitor the patient over time in order to determine whether the facial nerve will regain function. The patient should be followed clinically every 3 months to evaluate muscle recovery. EMG and nerve conduction studies can be used to predict facial nerve recovery.
Increasing weakness of facial function over time suggests a neoplastic process and needs to be investigated with that in mind.
Improvement of facial function over time needs to be followed clinically until stable. Once stable, reconstructive options can be considered.
Prior surgeries and treatments
Determine factors that may affect treatment plan. This would include: previous radiation, pre-existing anatomy, and previous reconstructive procedures.
Patient age and overall health
The selection of the reconstructive option is influenced by life expectancy of the patient, prognosis of the underline cause of paralysis, age, and overall health.
Specific patient complaints/concerns
Patient needs should be addressed.
Understanding the patient's specific aesthetic and functional concerns are the most important factors that guide the treatment. This will influence the extent and sequence of treatments for the eye, the mouth, or both.
3. Physical examination and documentation
A complete head and neck examination includes assessing for causes of facial paralysis (pathologies of the parotid or temporal bone).
It is essential to conduct a complete cranial nerve examination, with emphasis on V and VII.
Examination of Cranial Nerve (CN) V
Test the sensation of all the branches of CN V, with specific attention to corneal sensation.
Motor function: test active contraction of both the temporalis and masseter muscles (assessing for symmetry with the contralateral side), and normal mouth opening and clenching.
Examination of Cranial Nerve (CN) VII
The tone, strength, and coordination of the facial muscles are assessed on both sides for comparison. This includes an evaluation of synkinesis.
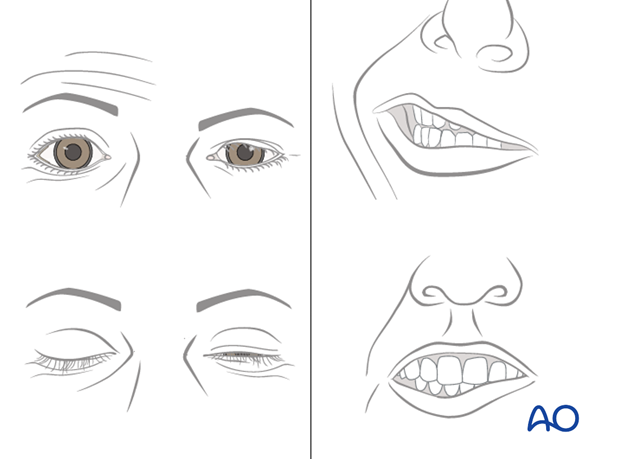
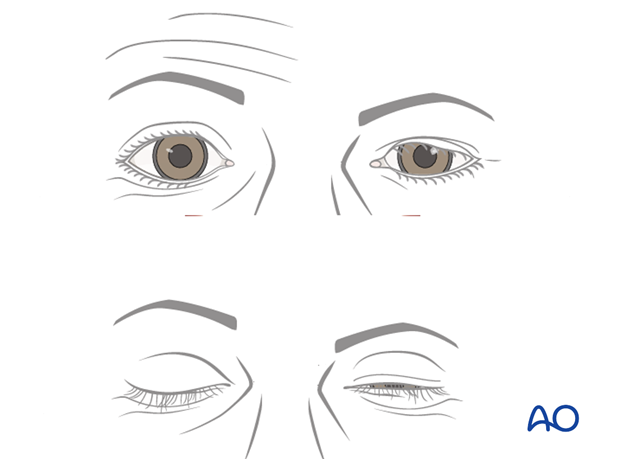
Each patient should be assessed for:
- Brow positioning and elevation
- Blinking and eyelid closure
- Bell's phenomena on eyelid closure
- Scleral show and ectropion of the lower lip
- Tearing, corneal irritation, and conjunctival injection
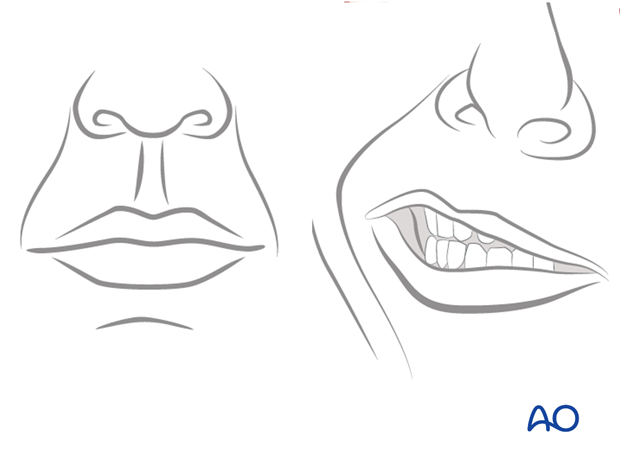
- Midface ptosis and presence of nasolabial fold at rest and during smile
- Nasal alar collapse and nasal airway
- Commissure and lip position during smile, pucker, and grimace
- Oral competence and speech
- Platysma and lower lip activity during rest and grimace (active lower lip depression)
Documentation
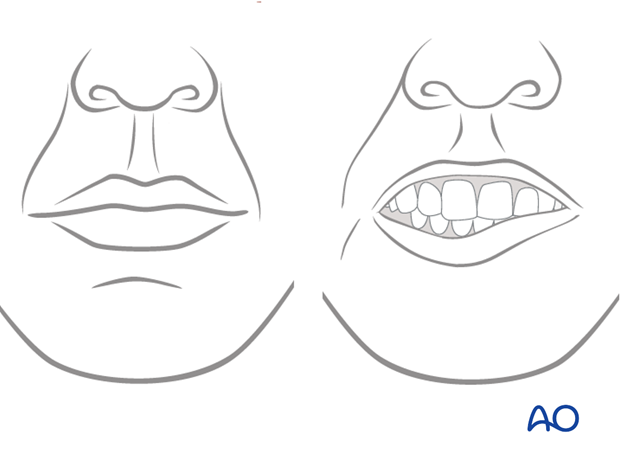
All patients should be documented with standardized photos and videos, at rest and with specific facial movements as described above.
This documentation should be performed at the initial examination and at subsequent follow-up visits, in order to better evaluate and determine muscle function, changes over time, and the result of the intervention.
Example of physical examination to assess facial nerve paralysis
4. Investigation
MRI/CT
High resolution cross-sectional imaging can be useful in numerous situations:
- Uncertainty of diagnosis, e.g. facial nerve schwannoma, neurotropic cancers
- Assessment of congenital facial paralysis
- Donor site evaluation, e.g. presence of plantaris longus tendon
EMG, nerve conduction studies
EMG and nerve conduction studies can be predictive of recovery and can be used as an adjunct to clinical assessment.
Intraoperative nerve stimulation and/or biopsy
In select cases, these investigations can help decision-making regarding nerve preservation and extent of nerve resection and reconstruction.
5. Patient expectations and motivation
Patient needs should be addressed. Understanding the patient's specific aesthetic and functional concerns are the most important factors that guide treatment. This will influence the extent and sequence of treatment of the eye, the mouth, or both.
Patient motivation will affect the type of reconstruction performed, the extent of reconstruction, recovery, and postoperative rehabilitation.
It is critical to gauge the motivation of the individual patient, because this will influence the quality of the outcome, especially in dynamic reconstruction.













