Radial forearm
1. Introduction
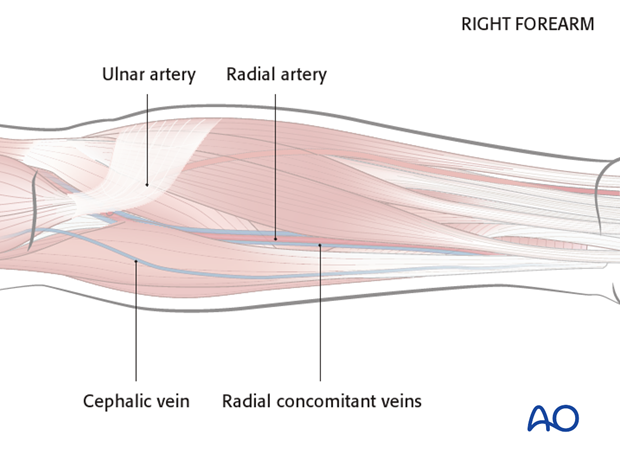
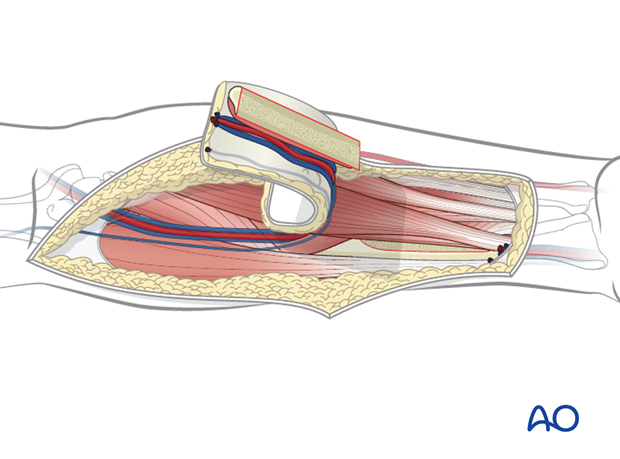
Anatomy
The blood supply of the flap is based on the radial artery, radial concomitant veins (deep system) and the cephalic vein (superficial system).
The following landmarks should be identified and marked prior to surgery:
- The radial artery (identified by palpation)
- The cephalic vein
Flap design
The flap can be harvested in a size up to 8 x 16 cm.
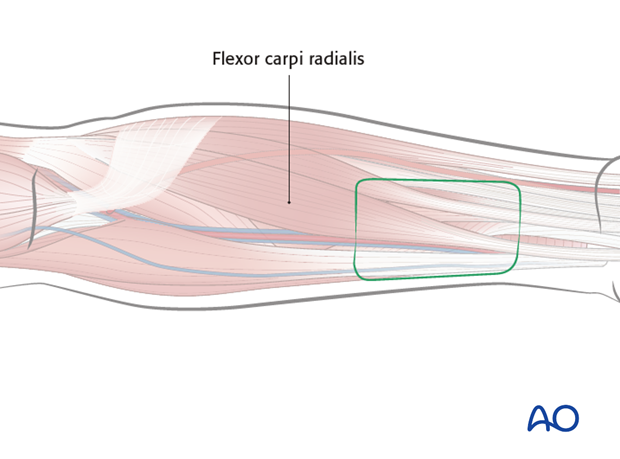
The flap should be centered between the cephalic vein (if this vein is to be used) and the radial artery. If cephalic is not reliable or if radial venae comitantes are selected, the flap will be centered at radial artery.
The palmar border of the flap should be placed over the flexor carpi radialis.
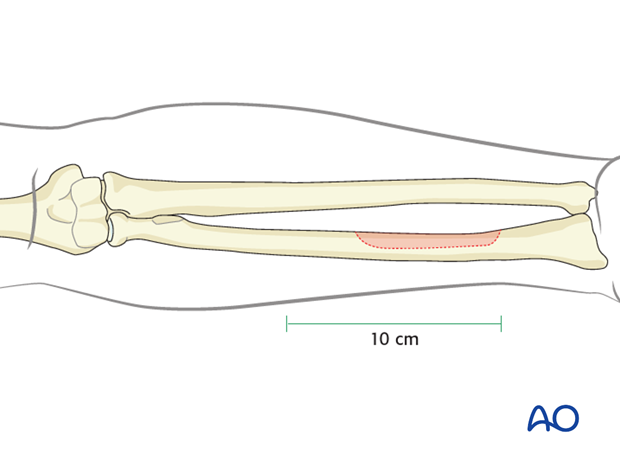
When bone is harvested the maximum length will be 10 cm. The maximum width of the radial bone is 45 % of the circumference.
It is limited by the wrist distally and the insertion of the pronator teres muscles proximally.
2. Flap harvest
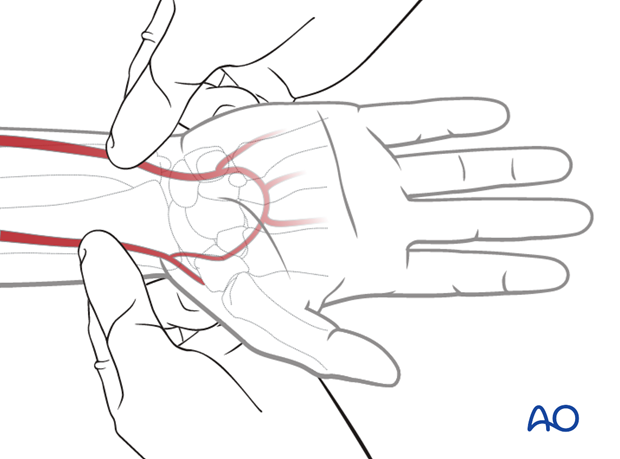
Allen's test
An Allen's test is performed to ensure the integrity of the palmar circulation prior to the harvest of the radial forearm flap.
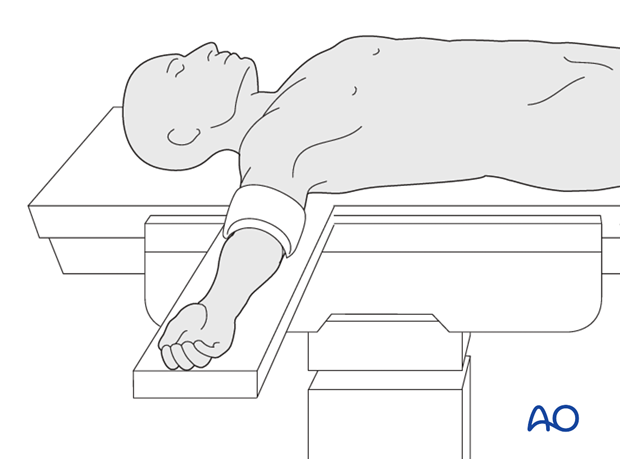
Placement of tourniquet
A tourniquet is placed on the upper arm and inflated to a pressure of 1.5x patient’s systolic pressure (usually 250 mmHg). The tourniquet should not be applied for more than 60 min.
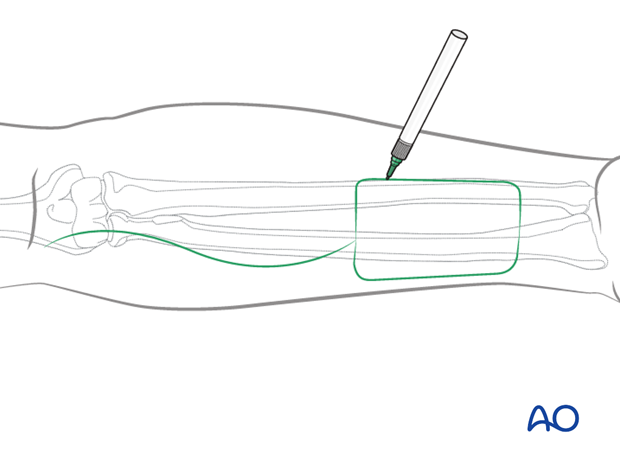
Flap outline
The flap outline is marked on the skin together with a proximal wavy line, 1 cm away from the antebrachial fossa.
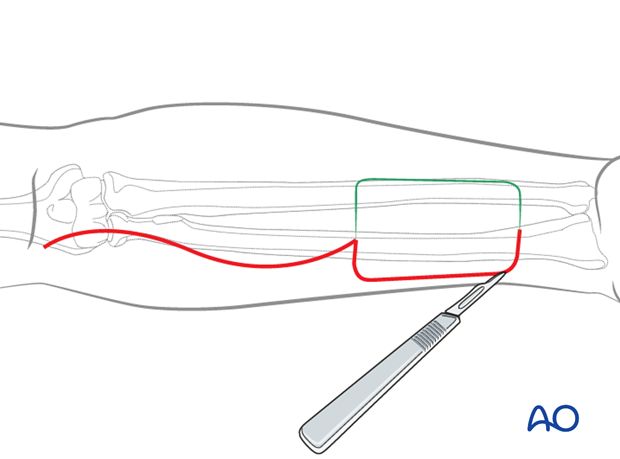
Skin incision
The skin incision is performed as outlined.
Lateral incisions can be carried down to the deep fascia of the skin taking care to keep underlying paratenon intact.
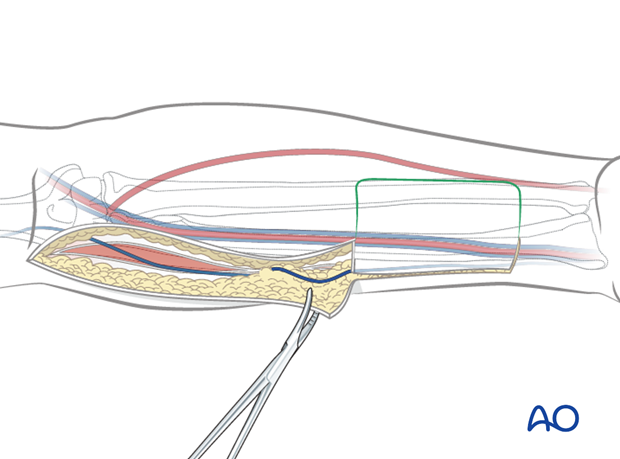
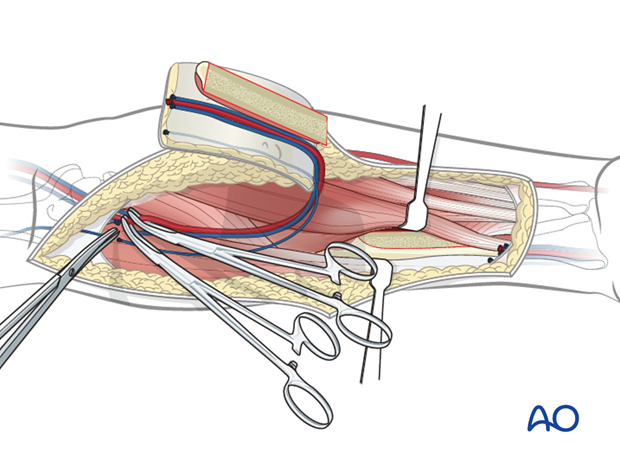
Mobilization of cephalic vein
The wavy skin incision is made down to the subcutaneous tissues and raised laterally, the cephalic vein is identified.
Dissection continues lateral to this through the fascia down to the brachioradialis muscle.
The flap and fascia are elevated towards the vascular bundle to the medial edge of the brachioradialis muscle along its entire length.
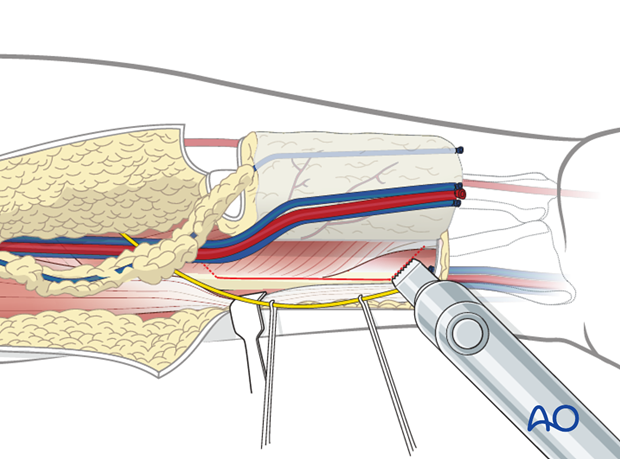
Ligation of distal vessels
Blunt dissection for the cephalic vein, radial artery, concomitant veins is performed at the distal end of the flap.
The distal end of the cephalic vein, radial artery and radial vein are transected and ligated.
The superficial branches of the radial nerve are identified and preserved.
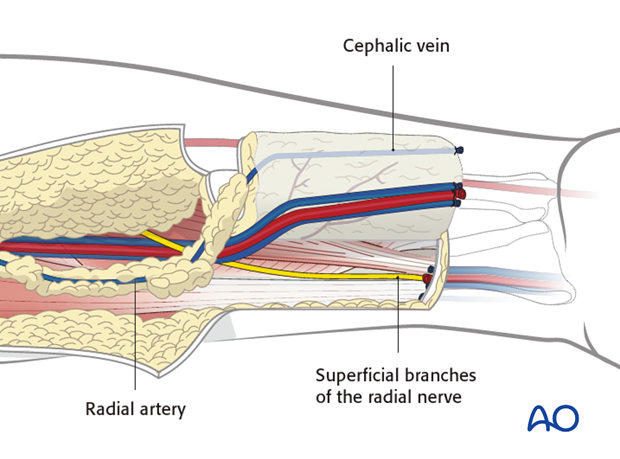
The brachioradialis muscle is retracted laterally and the edge of the radial bone is identified.
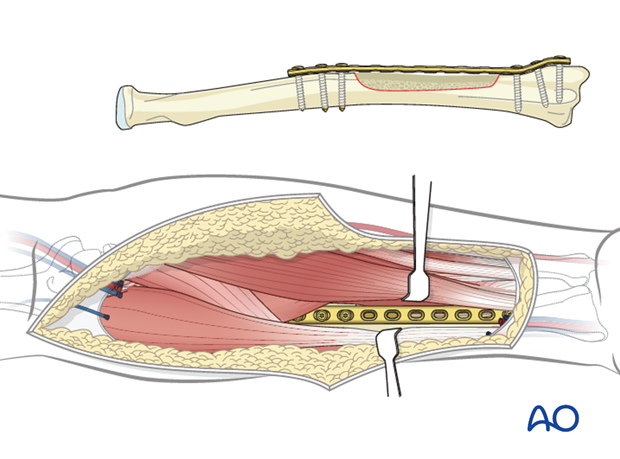
The periosteum is incised along the radial bone at 50% of its thickness.
Full thickness radial bone should be left at the wrist to allow for 2-3 screws of a reconstruction plate.
Dissection proximally should not go beyond the insertion of the pronator muscle.
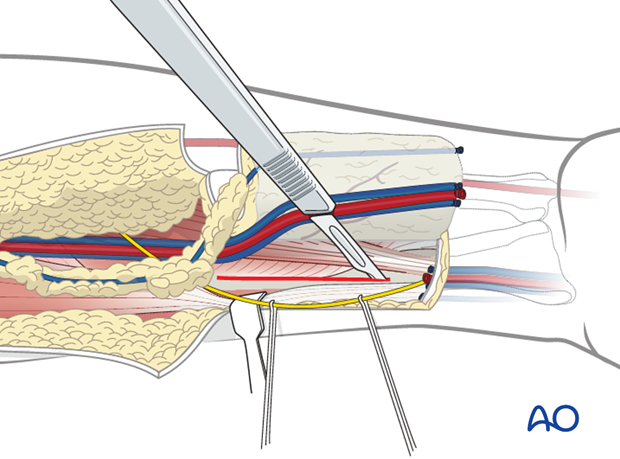
Utilizing a sagittal saw, an osteotomy is performed at the radius approximately at 50% of its thickness.
At the distal and proximal end of the osteotomy the bone cut should be made in an oblique fashion.
The flexor pollicis longus muscle is incised with an electric cautery at the medial extent of the osteotomy.
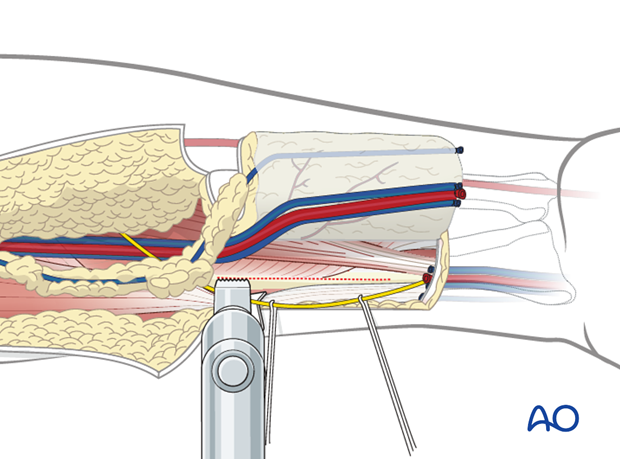
Dissection now continues through the soft tissues of the ulnar side of the flap. Dissection continues down to the palmaris longus tendon and flexor carpi radialis muscle.
The fascia is then elevated to the medial aspect of the flexor.
The soft tissue and bone are elevated in a distal to proximal direction. A cuff of flexor pollicis muscle is kept with the bone to maintain its vascularity.
At the proximal edge of the bone harvest, the dissection of the flap continues exactly as one would for a soft tissue only flap.
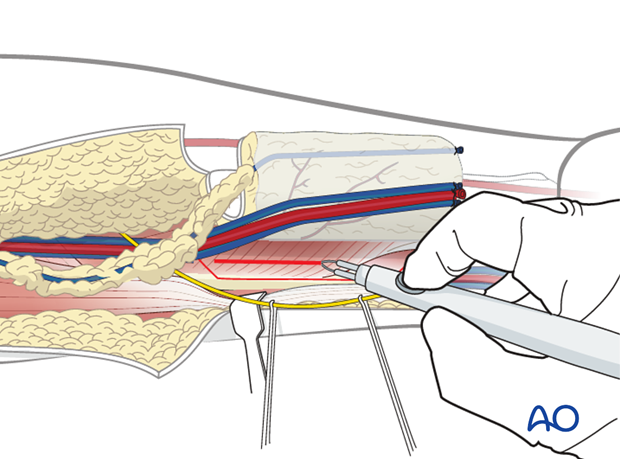
Mobilization of vascular bundle
The brachioradialis is retracted laterally and the vascular bundle located in the groove between the brachioradialis and flexor carpi radialis muscles is mobilized taking care that all its branches (perforators to the muscles) are ligated.
The pedicle dissection along the intermuscular septum is continued to the level of the brachial artery. The flap is then re-perfused by releasing the tourniquet to verify the viability of the fasciocutaneous flap.
In addition it is important to also assess the vascularity of the hand at this point.
Hemostasis is obtained and the vascular pedicle is then divided when the recipient site is ready.
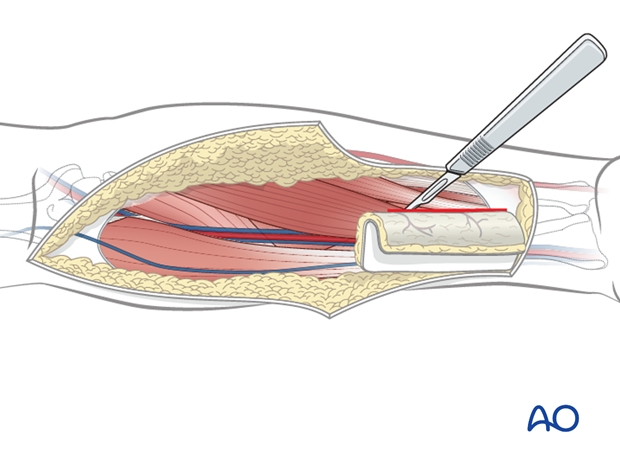
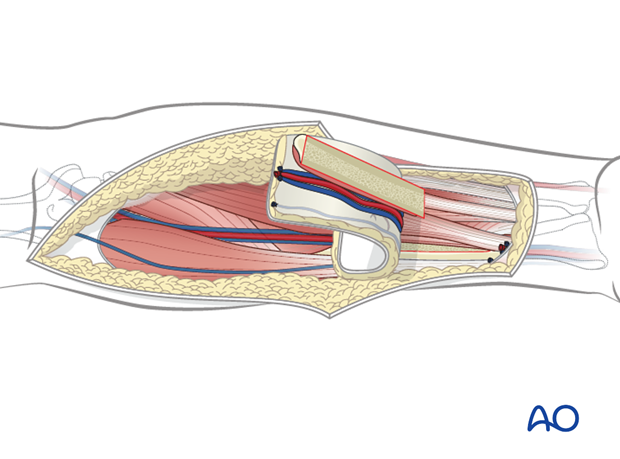
Closure
In order to minimize the risk of radial bone fracture, a reconstruction plate is placed to bridge the bony defect. Ideally 3 holes beyond each end of the bone cut should be placed for plate stability.
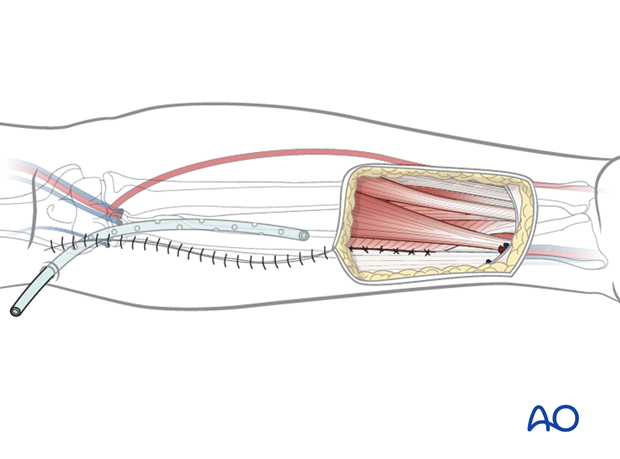
The edge of the flexor pollicis longus muscle should be sutured to the medial edge of the brachioradialis muscle to completely the cover the reconstruction plate.
A suction drain should be placed in the proximal aspect of the wound exiting through a separate stab incision at the antecubital fossa.
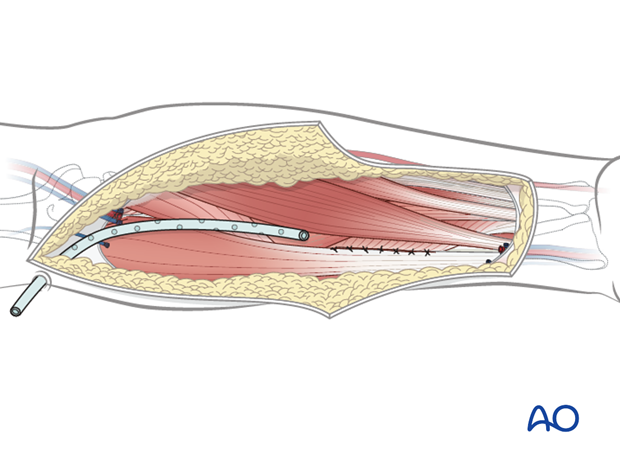
The proximal portion of the wound should be closed in layers leaving the distal forearm defect from the flap harvest.
A split thickness skin graft (0.18 inch thickness) is applied to the distal forearm defect. Fenestrations are placed in the graft.
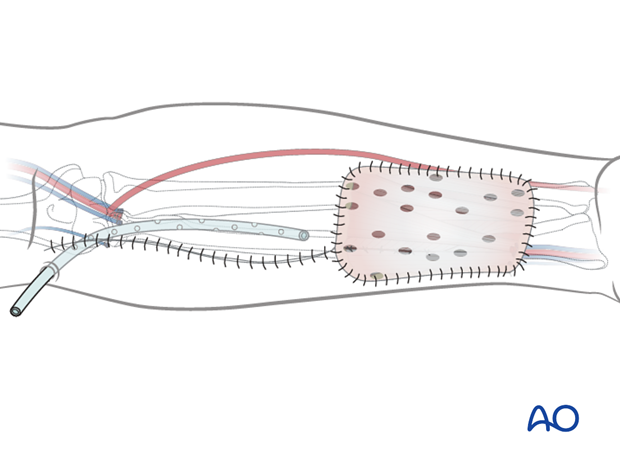
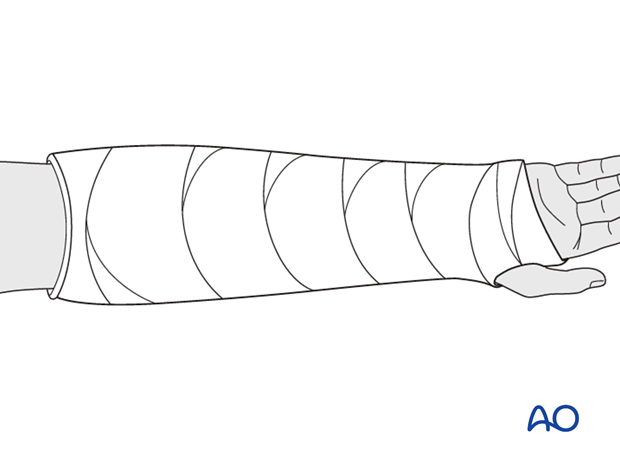
A volar forearm splint is placed for seven days.