Submandibular approach
1. Introduction
This approach is selected for access to the angle and ascending ramus in selected cases when a transoral approach is not appropriate.
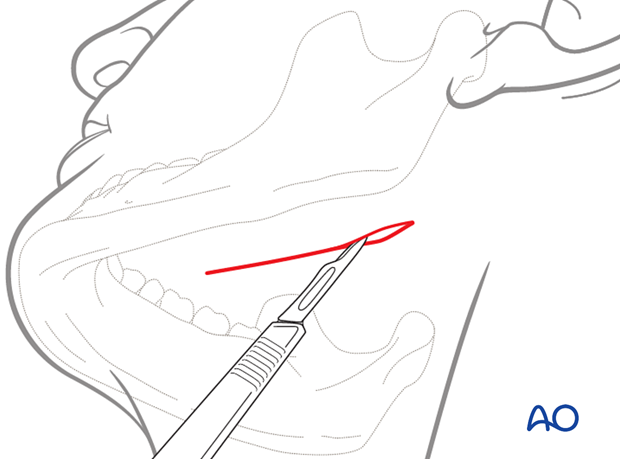
If using skin creases for the incision the orientation of the scalpel blade is parallel to the relaxed skin tension lines (RSTL).
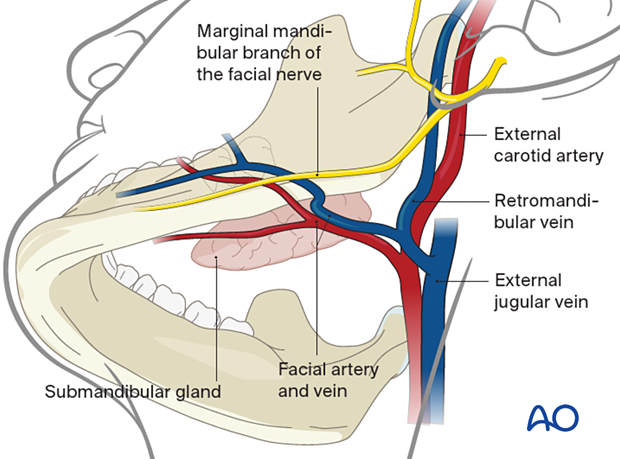
Neurovascular structures
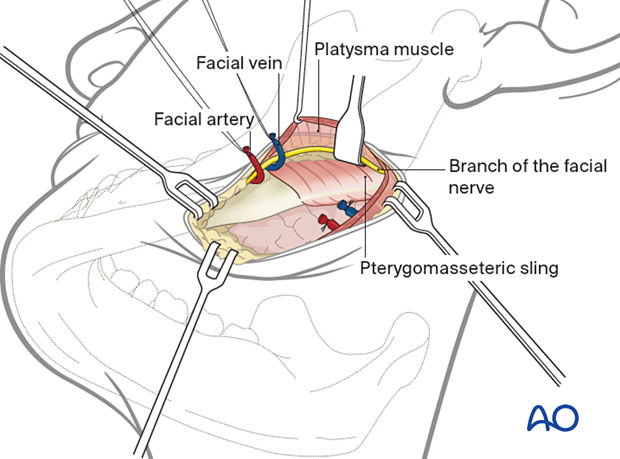
The main neural structure is the marginal mandibular branch of the facial nerve (CN VII). The facial artery and vein can also be encountered during this dissection.
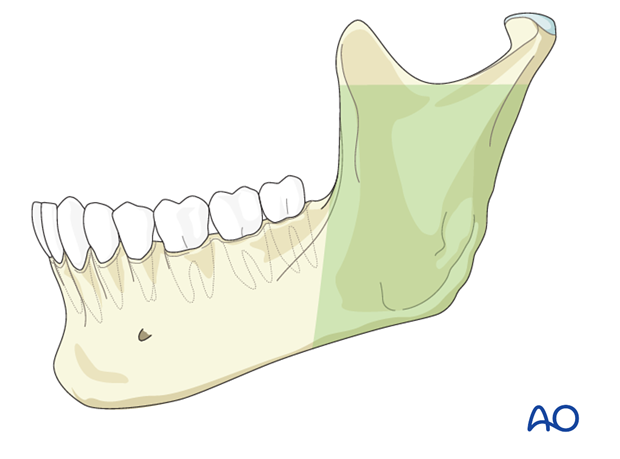
Exposure offered by the submandibular approach.
2. Skin incision
General consideration
Unless contraindicated, infiltrate the area with a local anesthetic containing a vasoconstrictor.
Use of a local anesthetic containing a vasoconstrictor may impair the function of the marginal mandibular nerve and prevent the use of a nerve stimulator during the surgical procedure. Therefore, consideration should be given to using a physiological solution with vasoconstrictor alone or injecting the local anesthetic with vasoconstrictor in a very superficial manner.
Muscle relaxants can also impair nerve function and must be taken into account.
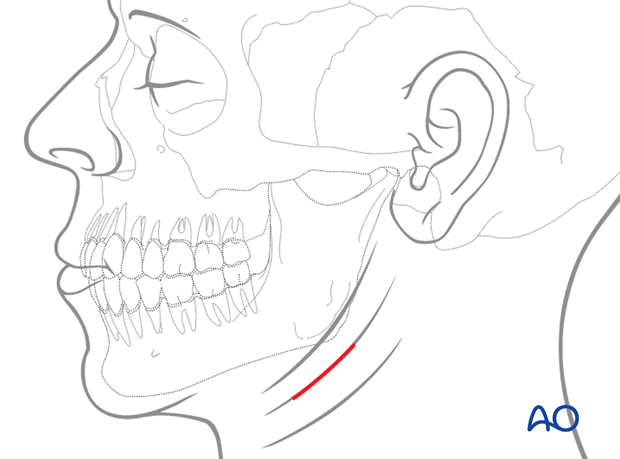
The length of the incision depends on the design of the osteotomy and the planned internal fixation technique. It should be kept as short as possible. Diagram shows a skin incision 2-3 cm below the inferior border of the mandible.
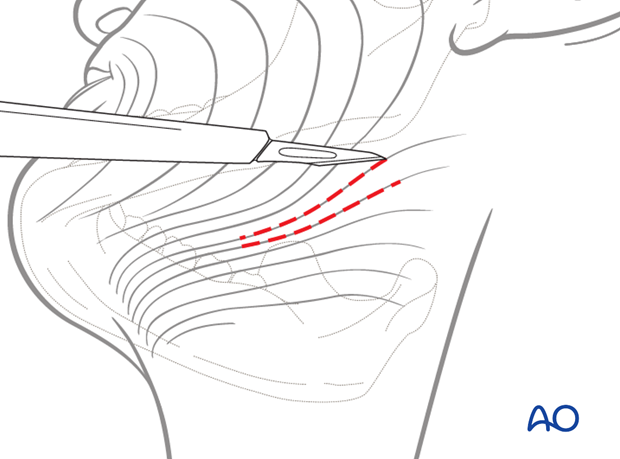
Incision of skin and subcutaneous tissues exposes the underlying platysma muscle.
3. Dissection
In order to protect the marginal mandibular branch of the facial nerve, the platysma is undermined bluntly with scissors prior to dividing it with a scalpel.
The platysma muscle is divided sharply, preferably 2-3 cm below the mandibular border, not necessarily at the same level of the skin incision.
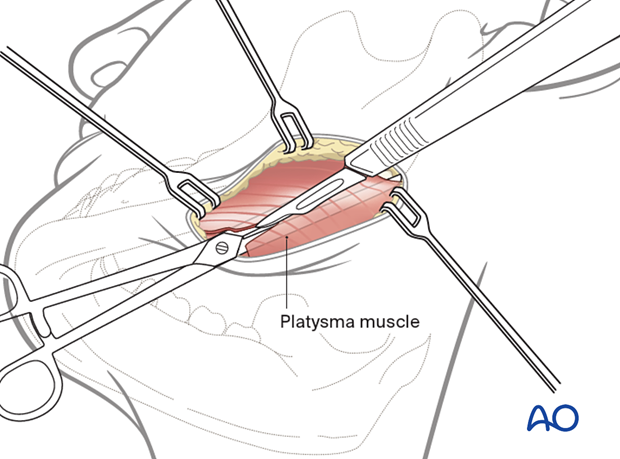
Superior subplatysmal dissection would expose the underlying marginal mandibular branch of the facial nerve (CN VII). This is not usually necessary.
If ligation of the facial artery and vein is necessary, the retraction of the vessels superiorly protects the marginal mandibular branch of the facial nerve, which usually lay superficial to the facial vein.
4. Exposure
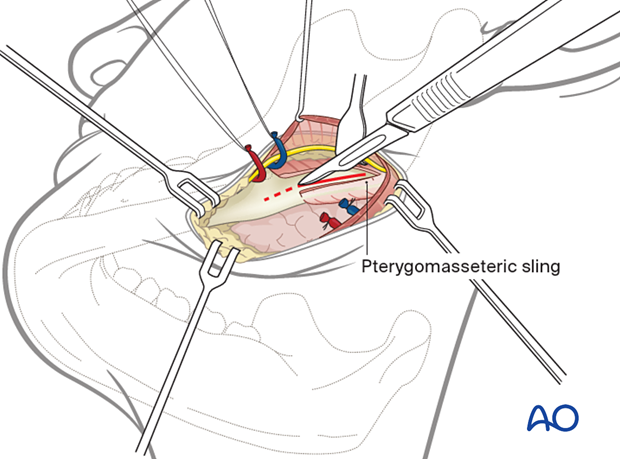
Divide the pterygomasseteric sling and incise the periosteum at the inferior border to expose the ramus.
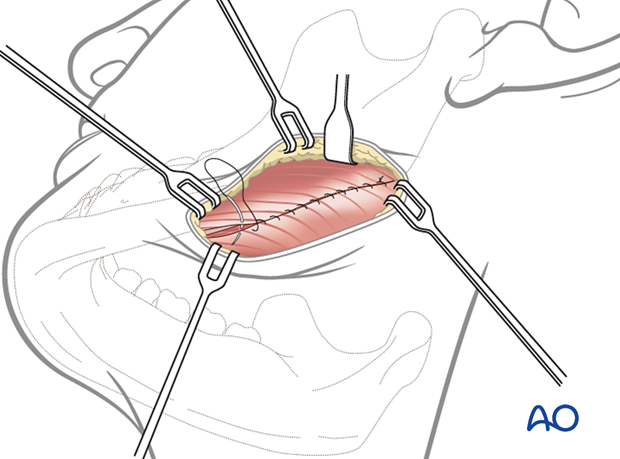
5. Wound closure
During wound closure, the pterygomasseteric sling is closed.

The wound is then closed in layers to realign the anatomic structures and eliminate dead space. The platysma muscle is closed. A variety of skin closure techniques are available based on surgical preference. A drain may be used if necessary.