Lateral eyebrow approach
1. General considerations
The lateral eyebrow approach provides a simple and rapid access to the superolateral orbital rim. No functionally important neurovascular structures are at risk in this approach.
2. Vasoconstriction
Subcutaneous infiltration of a local anesthetic/vasoconstrictor solution of the soft tissues overlying the superolateral orbital rim is helpful for hemostasis.
3. Protection of the globe
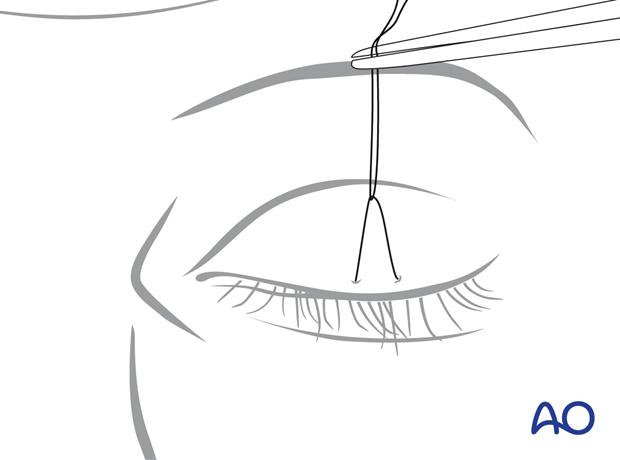
The cornea is protected with a temporary tarsorrhaphy or with a corneal shield.
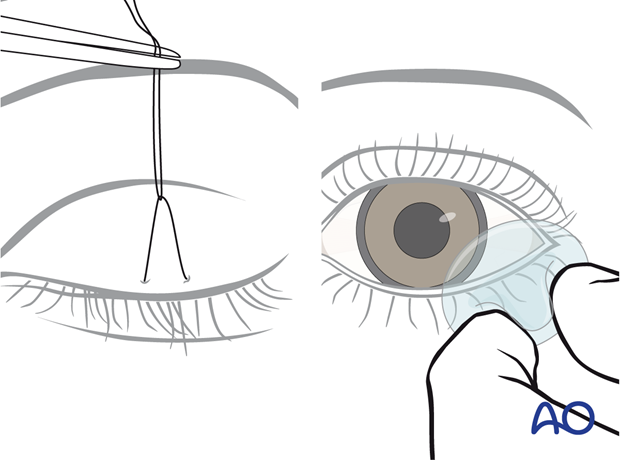
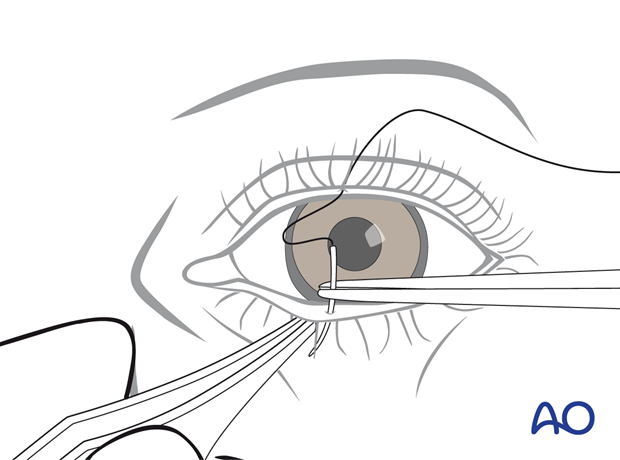
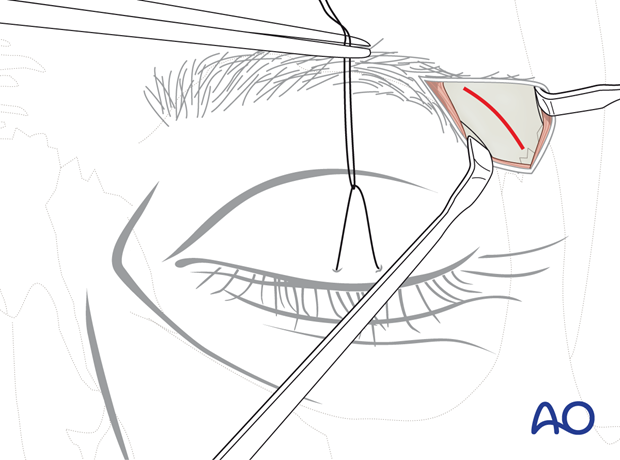
Below, the steps of a temporary tarsorrhaphy are shown.
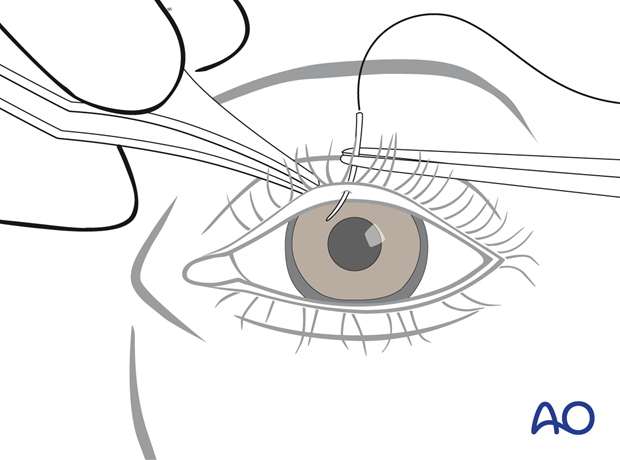
The needle is passed in the lower eyelid from the Gray line into the skin where it exits.
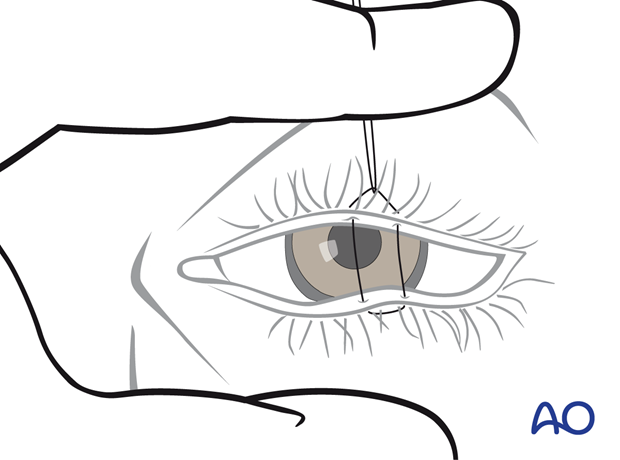
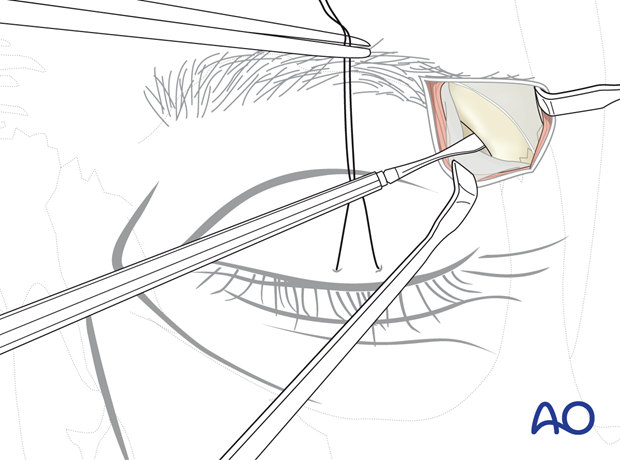
The suture is guided back, picking up the same soft-tissue portions in the lower and upper eyelids to complete the mattress loop.
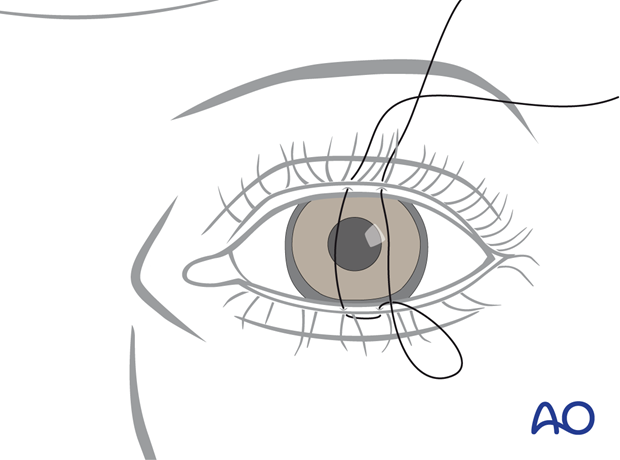
The tarsorrhaphy is not secured tightly, and some space is left between the knot and the upper-eyelid skin. A hemostatic clamp is used to grasp the suture and apply traction to the lower lid for full eyelid closure during the surgical procedure.
Since the suture was not fully tightened, when the hemostatic clamp is released, the lid may be opened for a forced duction test or evaluation of the pupil during the procedure.
4. Skin incision
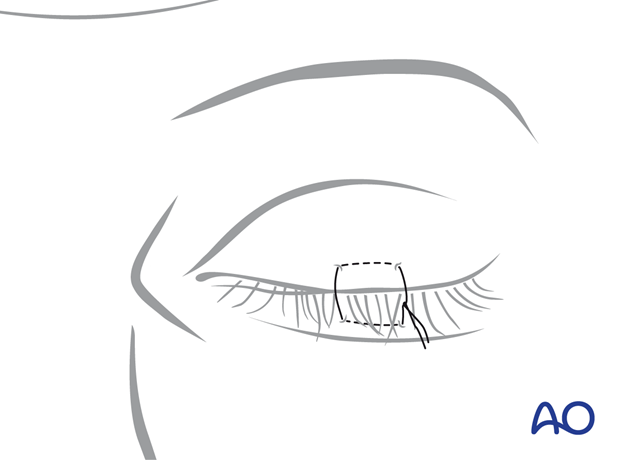
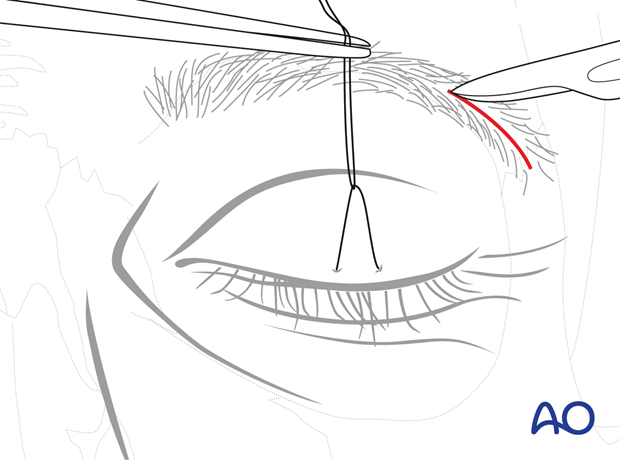
Before the incision, the lateral eyebrow hair is moistened and parted to open a line for the planned incision. An approximately 2 cm long horizontal incision is marked within the bounds of the lateral eyebrow parallel to the hair follicles. The incision goes through the skin first and then through the subcutaneous fat and muscular tissue layers.
Care is taken not to injure the hair follicles during the incision.
The orbicularis oculi muscle is undermined at a level below the retro-orbicularis oculi fat to expose the supra-periosteal plane.
The wound edges become freely moveable by the supraperiosteal dissection and are retracted over the zygomaticofrontal suture or the fracture area.
5. Periosteal incision
The periosteum is exposed and split sharply with a scalpel along the middle of the superolateral orbital rim.
6. Subperiosteal dissection of the superolateral orbital rim and internal orbit quadrant
The underlying bony structures are freed using sharp periosteal elevators.
The medial surface of the superolateral orbital rim is exposed first to gain entrance to the fossa of the lacrimal gland. Starting the subperiosteal dissection from within this bony concavity inside the anterolateral portion of the orbital roof, the periosteal envelope can be stripped off with ease from the superolateral orbital rim and the adjacent intraorbital quadrant.
Exposure to the lower portion of the lateral orbital rim is facilitated by a wide undermining of the skin and periosteum.
7. Closure
Wound closure is performed in three layers (periosteum, subcutaneous connective tissue, and skin).













